Urinary Tract infection Revision cards
- Created by: dboyd747
- Created on: 21-03-22 15:48
what is a Urinary Tract Infection?
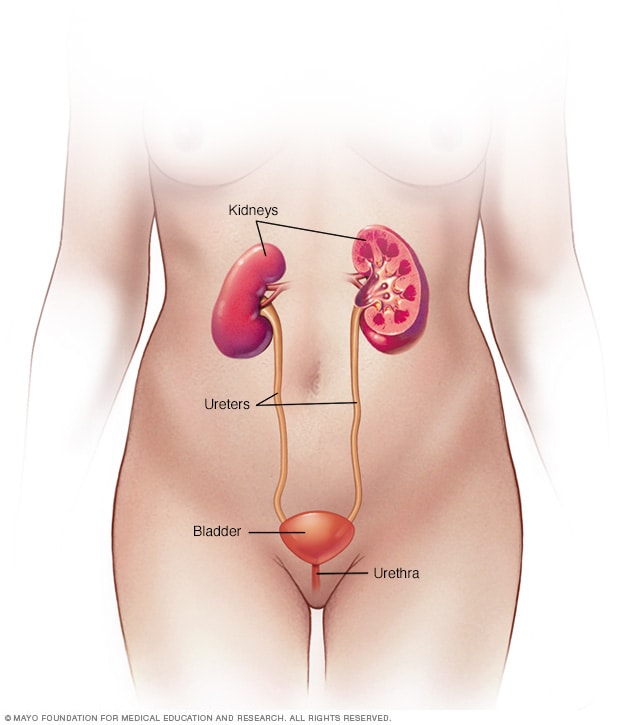
- A Urinary tract infection, or UTI, is an infection in any part of your urinary system, which includes your kidneys, bladder, ureters, andurethra.
- If you're a woman, your chance of getting a urinary tract infection is high. Experts rank your lifetime risk of getting one as high as 1 in 2, with many women having repeat infections. About 1 in 10 men will get a UTI in their lifetime
Types of UTI'S
An infection can happen in different parts of your urinary tract. Each type has a different name, based on where it is.
- cystitis (bladder): You might feel like you need to pee a lot, or it might hurt when you pee. You might also have lower belly pain and cloudy or bloody urine.
- Pyelonephritis (kidneys): This can cause fever, chills, nausea, vomiting, and pain in your upper back or side.
- Urethritis (urethra): This can cause a discharge and burning when you pee
Key diagnostic factors
Dysuria: Experiences a burning pain when passing urine. Dysuria is 1 of the 3 key diagnostic signs and symptoms of UTI in women aged under 65 years without a catheter (along with new nocturia and cloudy-looking urine).
New nocturia:Passing urine more often than usual at night.New nocturia is 1 of the 3 key diagnostic signs and symptoms of UTI in women under 65 years without a catheter (along with dysuria and cloudy-looking urine).New nocturia may be a sign of other problems, such as urinary retention and diabetes.
Cloudy-looking urine: Urine is cloudy to the naked eye. Cloudy-looking urine is 1 of the 3 key diagnostic signs/symptoms of UTI in women under 65 years without a catheter (along with dysuria and new nocturia).
Fever:In women aged under 65 years, a temperature of ≥37.9°C may indicate pyelonephritis or sepsis.
**The most common symptom is fever but this is non-specific. The absence of a fever does not exclude a UTI.
Other common signs & symptoms
Urgency: Urgency in women aged under 65 years and new urgency in women over 65 years is a common symptom that can indicate a UTI. It can also be a sign of an overactive bladder.
Visible haematuria: In women aged under 65 years, visible haematuria can be an indication for UTI. However, when it is a finding on its own, consider causes other than a UTI and investigate as appropriate.
Frequency: This is a common symptom that can indicate a UTI
Suprapubic pain or tenderness: This increases the probability of an UTI.
Flank pain: Can be a sign of a kidney problem - many organs are in this area, other causes are possible. Flank pain and fever, chills, blood in the urine, or frequent or urgent urination, then a kidney problem is the likely cause. It could also be a sign of kidney stones.
New incontinence: In women aged over 65 years, this can indicate a UTI when combined with another symptom.
New or worsening delirium/ debility: In women aged over 65 years, this can indicate a UTI when combined with another symptom in this group. Also consider other causes of delirium (use the PINCH ME mnemonic - pain, other infection, poor nutrition, constipation, poor hydration, other medications, environment change).
Risk factors – strong
- Sexual activity: Sexual intercourse is the strongest risk factor. Any lifetime sexual activity and any sexual activity during the past year are strongly associated with recurrent UTI.
- Spermicide use: Spermicides, decrease vaginal lactobacilli, which facilitates vaginal Escherichia coli colonisation and results in an increased risk of UTI. Even the relatively small amounts of spermicide coating condoms increases the risk of UTI.
- Post menopause: The absence of oestrogen (consistent with urogenital atrophy, vaginal atrophy, and also known as genitourinary syndrome of menopause) is a risk factor for UTIs.
- Positive family history of UTIs: Having a mother with a history of UTIs is associated with a two- to fourfold increase in risk of recurrent UTI
- History of recurrent UTI: A well-established risk factor.
- Presence of a foreign body: Any indwelling catheter or any foreign body (stone, suture, surgical material, or exposed polypropylene mesh from pelvic surgery) significantly increases risk for UTI. Foreign bodies serve as nidus for UTIs and interfere with a person's ability to clear a UTI.
**Bacteriuria occurs in the presence of indwelling or intermittent catheters, and asymptomatic bacteriuria does not require treatment. When a symptomatic UTI is present in a patient with a catheter or stent, catheter or stent change should be strongly considered
Risk factors - weak
Insulin-treated diabetes: Considered a more predominant risk factor in older women. High lifetime number of UTIs.
Recent antibiotics: The recent use of certain antimicrobials may predispose women to UTIs through their effects on the genitourinary microbiome.
Poor bladder emptying: Due to either poor detrusor muscle contraction or bladder outlet obstruction (e.g., secondary to pelvic organ prolapse or a prior anti-incontinence procedure), can lead to urinary stasis, interfering with a person's intrinsic ability to clear bacteriuria.
Increasing age: 10% women >70 year have UTIs.
Key clinical manifestations
- Dysuria: Results from irritation of the bladder trigone or urethra. Inflammation or stricture of the urethra causes difficulties starting urination and burning on urinating.Urine comes in contact with inflamed mucosa. Nociceptors and sensory nerves stimulated which causes pain along with burning, stinging or itching
- Frequency, urgency & incomplete voiding: Reduced bladder capacity due to inflammatory oedema causing decreased compliance and pain due to bladder distension.
- Cloudy urine: Typically comes from discharge of either pus or blood into the urinary tract – potentially also be a build-up of white blood cells as body tries to eliminate invading bacteria
- No fever: If fever was present: normally, the hypothalamic thermoregulatory centre maintains the internal temperature between 37° and 38° C.
Fever results when something raises the hypothalamic set point, triggering vasoconstriction and shunting of blood from the periphery to decrease heat loss; sometimes shivering, which increases heat production, is induced. These processes continue until the temperature of the blood bathing the hypothalamus reaches the new set point. Resetting the hypothalamic set point downward (eg, with antipyretic drugs) initiates heat loss through sweating and vasodilation.
**Pyrogens are substances that cause fever. Exogenous pyrogens are usually microbes or their products. Fever is the result of exogenous pyrogens that induce release of endogenous pyrogens.
continuation: Key clinical manifestations
No flank pain- If present: caused by distention of the ureter or renal pelvis or distention of the renal capsule, due to inflammatory response following infection
Pathophysiology- The most common route of infection in females is via an ascending pathway. Colonisation of the vagina may occur first, then ascends into the urinary tract. Ascending UTI is amplified by factors that promote the introduction of bacteria at the urethral meatus and by iatrogenic means. Stasis of bladder urine impairs the defence against infection provided by bladder emptying. While the mechanical model of ascending infection explains the means of onset of bacteriuria, host and bacterial factors explain the variability of risk for UTI among women.
Type 1 pili may enhance bacterial adherence and seem to be instrumental in the pathogenesis of bacterial cystitis. Type 1 piliated Escherichia coli bind in greater numbers to vaginal fluid from women with E coli vaginal colonisation. Alkalinisation of vaginal fluid (as occurs post-menopausally) results in augmented binding. Conversely, acidification of vaginal fluid pH by application of topical oestrogen compounds may reduce recurrence of UTI in post-menopausal women.


Comments
No comments have yet been made