Vital signs
- Created by: Charlotte170289
- Created on: 08-01-21 15:34
Why we record vital signs
- As nurses assessment, monitoring and interpretation is an essential role
- Consent should be gained before assessment is undertaken
- Each time we record vital signs, we are observing for physiological changes, so that we can intervene if necessary.
Assessment is the first process in the Nursing process, APIE:
- A- Assessment
- P- Plan
- I- Implementation
- E- Evaluation
Vital signs (NMC)
Annex B: nursing procedures clearly tells you what you are required to know to the point of qualification. This can be found on page 33 of the future nurse: standards of proficiency for registered nurses.
2. Use evidence-based, best practive approaches to undertake the following procedures:
- take, record and interpret vital signs manually and via technological devices
- Undertake a whole body systems assessment including respiratory, circulatory, neurological, musculoskeletal, cardiovascular and skin status
- Measure and interpret blood glucose levels
- Undertake, respond to and interpret neurological observations and assessments
What are vital signs
They are fundamental skills used in the care of all patients:
- Blood pressure
- Pulse rate
- Respirations
- Capillary refill time (CRT)
- Oxygen saturations (peripheral O2 saturations)
- AVPU - (Alert, verbal, pain, unresponsive)
- Capillary blood glucose
- Temperature
- Urine output
We all have vital signs
Regardless of the following factors:
- Age- children have different parameters based on age groups
- Gender
- Fitness level- athletes are known to have lower blood pressure and pulse rates
- Illnesses/injury/trauma
- Ethnicities
- Disabilities
- Medications- Illegal or legal
- Food and fluid intake (diet)
- Weight- Obesity and low weight can affect vital signs too
Vital signs are checked when;
- We do initial assessments, to get a base line for comparison during admission
- A patient is ill, so that we can monitor for further potential deterioration and improvement
- Before, during and after patient surgery
- A patient is receiving a blood transfusion
- We want to check the suitability and effectiveness of treatment- evaluation
Scoring tool
- For adults we use NEWS 2 (National early warning score)
- Children- Adapted PEWS (paediatric early warning score)
- Mental health- You use an age appropriate vital sign scoring tool. You may also use other types of assessment tools in practice
- Learning disability- same as MH
- Midwifery- Obstetrics early warning score
NEWS 2
News 2 is a physiological track and trigger scoring system that provide early recognition of potential or established acute illness.
This scoring system, along with full assessment can lead to more successful patient outcome.
The 6 simple physiological parameters are:
- Respiratory rate
- Oxygen saturation
- Systolic blood pressure
- Pulse rate
- Levels of consciousness or new confusion
- Temperature
Vital sign- blood pressure
Cardiovascular system- blood presure
- Blood pressure is the force of blood against the walls of the arterial blood vessels. When the left ventricle contracts, blood is forced into the aorta. This increase in pressure is called Systole (first measurement in a blood pressure reading). When the heart relaxes, and the blood vessels subsequently relax, this is the diastole (second reading)
- Mean arterial pressure (MAP) is the pressure in the large arteries average over time. This value is important and is oftern displayed on automatic blood pressure machines. A mean arterial pressure of aound 60 mmHg is required for organ perfusion.
- Blood pressure results from cardiac output (CO) and systemic vascular resistance (SVR)
- BP= CO X SVR
- Blood pressure is affected by factors like circulation blood volume, blood vessel diameter, heart rate and contractility
What is blood pressure
- Cardiac output (CO) is the amount of blood pumped by the left ventricle into the aotra per minute. It is the indicator of blood flowing through peripheral veins. Cardiac output is affected by stroke volume and heart rate.
- CO= HR X SV
- Systemic vascular resistance (SVR) is dependant on the diameter (tone) of the arterial blood vessels. When blood vessels narrow, the SVR increases. This is known as vasconstricted. When blood vessels dilate, the SVR decreases ans we call this vasodilation.
- Stroke volume (SV) is the amount of blood ejected from a ventricle during a contraction. This affected by Preload, Contractility and Afterload.
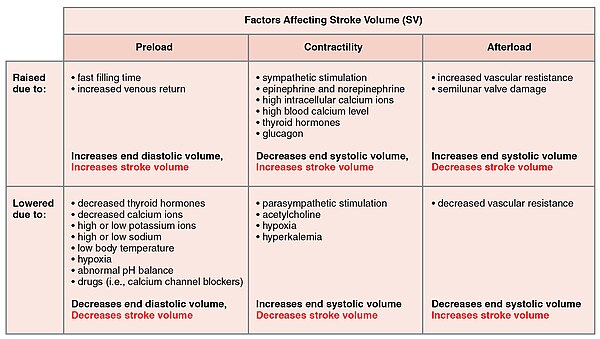
Preload, contractility, afterload
Preload is the stretch and recoil of the heart to get adequate blood volume pumped around the body. This is known as frank-starlings law of the heart (cardiac haemodynamics). If the heart does not get enough volume of blood through it, then it will not be sufficiently stretched to produce adequate recoil and so SV (stroke volume) will decrease.
Contractility is the force that the heart contracts. It is affected by the sympathetic nervous system, hormones, electrolytes and drugs. If the contractility of the heart is reduced or increased (as long as there is enough blood volume). The SV (stroke volume) will be affected.
Afterload is the pressure within the aorta and pulmonary artery and is directly affected by the volume of blood and resistance in the vascular system. Optimal afterload will eject a sufficient amount of SV (Stroke volume) with each contraction. However, if the afterload is higher than the pressure that is created by the actual contraction, then the SV (stroke volume) will be reduced.
Hormone response on BP
Angiotensin II creates vasoconstriction and stimulates aldosterone which assists in the reabsorption of water.
Atrial natriuretic peptide (ANP) released when atrium is overstretched. This causes vasodilation.
Adrenaline and norepinephrine produced in the adrenal cortex. They increase heart rate and contractility, cardiac output and blood vessel intergrity.
Antidiuretic hormone (ADH) from the hypothalamus and relased by the posterior pituitary gland when the concentration of blood solutes is affected. This causes urine output and vasoconstriction.
How we measure BP
We can measure blood pressure by:
- Aneroid sphyfmomanometer. This is the type of device used in manual blood pressure readings.
- Automatic blood pressure device
There are key sounds known as the korotkoff's that are vital when performing a manual blood pressure. These first thudding sounds called the first Korotkoff sound and indicate the value for the systolic blood pressure. The distinctive sounds, caused by tubulent arterial blood flow.
You record blood pressure readings in the "C" section of the NEWS chart.
Normal and abnormal BP
- A normal adult blood pressure will be between 110-140 mmHg systolic pressure and 70-80 mmHg diastolic pressure. Average blood pressure is less than 120 mmhG systolic.
- N.B. There are variations of what is considered normal and what is not.
- Whe is comes to children their systolic blood pressure is based on the stage of growth.
- Hypertension is generally a sustained blood pressure of above 140/90 mmHg
- Hypotention is generally classed as a BP of a systolic below 100 mmHg.
mmHg= millimeter of mercury
Performing BP reading
- When measuring the arterial blood pressure with sphygmomanometry and the use of a stethoscope (auscultation), the healthcare professional occludes the brachial artery with the inflated cuff. As the pressure is slowly released, a series of characteristic sounds—the Korotkoff sounds—can be heard, and noted against the graduated scale.
- Begin by palpating the brachial artery to confirm its position. If there is an arrow on the cuff, this must line up with the brachial artery. Make sure the cuff is at the level of the heart, whatever the position of the patient Before taking the arterial blood pressure with the stethoscope, estimate the systolic pressure. Palpate the brachial artery (or the radial artery if the brachial is hard to find) and rapidly inflate the cuff to 20 mmHg above the value where the pulse disappears
- Slowly deflate the cuff note the pressure where the pulse reappears; this is the approximate systolic pressure. Knowing this value will help you to locate the auscultatory gap when subsequently inflating the cuff and listening to the Korotkoff sounds. It also prevents unnecessarily high inflation of the cuff, which can be uncomfortable for the patient.
- Once you have estimated the systolic pressure through palpation, place the head of the stethoscope lightly over the brachial artery in the antecubital fossa. Deflate the cuff, using the valve on the bulb, at a steady rate of 2 mmHg per second, while keeping the head of the stethoscope on the antecubital fossa. You will hear the Korotkoff sounds as you slowly deflate the cuff
- Note the pressure when you first hear clear tapping sounds; this is the systolic pressure, K1. The pressure when the sounds become muffled is K4, the first diastolic pressure. The point when the last sound occurs is the second diastolic sound, or K5. Deflate the cuff slowly for a further 10–20 mmHg, checking that all sounds have disappeared. Then deflate the cuff quickly for the patient’s comfort. Repeat the procedure on the other arm. If there is a difference, use the higher value.
Vital signs- pulse
Cardiovascular system- pulse
- A pulse is generated when the left ventricle contracts. Oxygenated blood is pushed through the aorta, which created a pressure wave. This is the beat you feel when palpating a arterial pulse.
- Heart rate is the rate of the heart muscle. Pulse rate is the external indicator of the heart rate.
- So, if you palpate a pulse point for 1 minute and get 80 beats, you write 80 beats/min.

Affect of heart rate on cardiac output
- Cardiac output responds to changes in the metabolic demands of tissues associated with stress, exercise and illness. As we talked about last time, CO= SV X HR
- The heart rate is determined by the auto-rhythmic cells within the cardiac conductive system and is affected by the autonomic nervous system, drugs, hormones and electrolyets.
- Bradycardia suggests a low cardiac output. This results in organs and tissues potentially not receiving blood that contains oxygen and nutrients.
- Tachycardia increases cardiac output when the body has an increased demand for oxygen and nutrients (like during exercise or during pyrexia) However, when the tachycardia is so fast, that it spends less time in the relaxed stage of the cardiac cycle (diastole). Is the heart is so fast, that insufficient recoil of the heart, then cardiac output will be reduced.
- Changes in the heart rate are due to infibition or the stimulation of the sinoatrial (SA) node (hearts natural pacemaker) which is mediated by both the parasympathetic and the sympathetic areas of the autonomic nervous system.
- Heart rate is controlled by the balance of these 2 systems via signals that will either slow (parasympathetic) or speed up (sympathetic) the heart rate
- An increase in heart rate (sympathetic) usually occurs when the beta-1 receptior within the SA nodes are activated. This is a result of a release of catecholomines.
Receptors
Baroreceptors (in the aortic arch and inside both left and right carotid arteries) and the CNS affects the heart rate. Baroreceptors are sensitive to blood pressure changes. E.g. in hypertension, the baroreceptors release impulses to the cerebral medulla, which causes parasympathetic involvement which leads to lowering of both BP and heart rate.
In hypotension, parasympathetic response slows and sympatheric responses engage resulting in the elevation of BP (through vasoconstriction) and the heart rate increases too.
Pulse rhythm
Instigated by the cardiac conduction system and affects the cardiac cycle. Pulse rhythm is an indicator for heart rhythm. It can be regular, irregular, regularly irregularly and irregularly irregular.
Normal heart rate is sinus. The ventricle contracts at regular intervals.
If the pulse is regularly irregular, you will feel the pulse be regular but irregular.
If the pulse is irregularly irregular (like in atrial fibrillation) you will feel irregularities
Please remember that in some situations, a pulse may not be palpable if the ventricle contraction is not powerful enough to create the pressure wave. However, this would only be known if the pulse is felt while an electrocardiogram is done or if heart auscultation is being performed.
Pulse volume
The strength of the pulse is an indicator of the pressure of blood being exerted against the artery walls.
Terms used with pulse strength are: absent, weak, normal, increased or bounding.
The pulse can also be an indicator for assessing the blood pressure. There are debates about the actual mmHg that a pulse can be associated with, but a palpable radial pulse can mean a systolic blood pressre of around 70-80 mmHg. If a radial pulse is absent, but a carotid pulse (in the neck) or femoral artry is felt, the a blood pressure may be around 50-60 mmHg.
How we measure pulse
You must palpate a pulse that is nearest the skin- common and easiest to reach in adults are the Radial artery in the wrist and the Brachial artery in the crease of the elbow.
In children the brachial artery is the most accurate place.
When you are palpating the pulse you must note the following:
- Rate
- Rhythm
- Volume
Automated blood pressure machines do not pick necessary pick up arrythmias.
you would record the pulse on the cardiovascular part of the NEWS 2 chart
What is normal/ abnormal (Pulse)
Adult pulse ranges between 51-90 beats per minute
children- their hear rate are age dependent, but they tend to have a faster rate then adults between 60-180 BPM, they should not have a heart rate below 60 BPM
When palpating you may find that a patient may have a heart beat within those Normal ranges, but they have an irregular heart beat (must be escalated)
Any observations that is outside of normal will require attention. The NEWS 2 scoring system has been designed to assist clinicians in practice. The higher the score the more urgent the response.
Capillary refill time (CRT)
- CRT is the rate at which the capillaries (tiny blood vessels that connect veins and arteries) refill.
- It is another way in which we can assess the cardiovascular system- mostly done in children as a vital sign, but should be done in the adult person too.
- It can be performed in any setting. It can be done when someone has a plaster cast on a limb- you should record the CRT on all of these patients as a cast that is too tight has the potential to compromise circulation to toes and fingers.
- In both adults and children patients, a normal CRT is less than 2 seconds
- In children the CRT is a good quick assessment of shock. The ideal place for a CRT is the sternum on the chest.
- One the PEWS chart- there is usually a specific space that states more than 2 seconds or less than 2 seconds and an appropriate score will be given to the result.
- In adults this can be done, although the most common place is the nail bed.
- On the NEWS 2 there is no specific are for the CRT- some staff will create an area, some will just record it in the notes.
Respiratory and O2
The respiratory system provides the cells within the body with oxygen and removes carbon dioxide.
Breathing is expressed as inspiration (in) and expiration (out). There are 4 processes:
- Pulmonary ventilation- where movement of air in and out of the lungs is done to refresh gases
- External respirations- is commonly referred to as gaseous exchange
- Transport of respiratory gases- is oxygen from the lunds to cells, and carbon dioxide from cells to the lungs. This is accomplished by the cardiovascular system.
- Internal respiration- is the movement of oxygen from blood into cells and carbon dioxide from cells into the blood.
Normal V/Q- unoxygenated blood goes fom the venous system and into the right side of the heart (through the pulmonary artery into the lungs, where is has carbon dioxide). The arteries branch off into the alveoli capillaries which is where the gas exchange occurs.
The 2 areas we measure:
- respirations (RESPS)
- oxygen saturations (SATS)
Gas exchange- external res
- Gaseous exhange is the exchange of O2 and Co2. This exchange occurs in the alveoli and our blood. Alveoli are little air filled sacs that responds to the gaseous exchange.
- Alveoli have greater surface area to volume ration which allows for the gas exchange
Partial pressure gradient
- Oxygen partial pressure gradient is about 60 mmHg (100mmHg in alveolar air and 40mmHg in deocygenated blood)
- O2 diffuses quickly from the alveolar air into the capillary
Oxygen
- Control of respiration primarily occurs in the medulla and pons (in the brainstem)
- Oxygen consumption increases exponetially when the body is exercising or during ill health. There are several reasons mechanism that help to keep up with the metabolic demands in the cells. These include higher brain centers, chemoreceptors and reflexes that occurs in the brainstem.
- Oxygen is carried in the blood and is attached to haemoglobin. This is called oxyhaemaglobin. Oxygen saturation is a measure of how much oxygen is being carries as a % of the maximum it can carry.
- One haemoglobin molecule can carrt a maximum of 4 molecules. So if a patient is carrying 3 out of 4 molecules of oxygen we could say that they have a 75%. However a patient who has 75% oxygen would be unwell
- So in relation to SPO2 and the large number of haemoglobin molecules the result of SPO2 is higher.
Common causes of resp issues
- Pneumonia
- Chest infections
- Pulmonary oedema (fluid in the lungs)
- Chronic respiratory disease (chronic obstructive pulmonary disease)
- Asthma
- Remember that respiratory failure may be a result of other systemic issues like stroke, muscular degenerative disease and sepsis
How to measure Resps
- Respirations are recorded as a number and we count them by watching the patient.
- You should observe the patient for the following:
- Colour of the patient- in hypoxia (low O2 levels) blue discoloration (cyanosis) occurs around the lips and eye lids
- Respiratory rate and movement of the chest
- How deep the person breathes- shallowly or deeply
- For a cough, and noises like wheezing or rattling, other noises may suggest an airway obstruction.
- On the adult NEWS 2 chart there are 2 sperate areas for non COPD and COPD
- Respiratory failure is when oxygen levels are too low and/or carbon dioxide levels are too high. If a patient has low oxygen and their respiratory rate is high, they are likely to tire very quickly
Pulse oximetry
Pulse oximetry is the way in which we assess and measure a patients oxygen saturations. This is expressed as a SpO2.
Oxygen is recorded as a percentage
Be mindful that pulase oximetry can be affected by certain conditions:
- Anemia
- Nail varnish
- cold peripheriers
- High carbon dioxide levels- hypercapnia. These are not detected via spo2 monitoring
Cyanosis is a sign that oxygen levels are low and oxygen supplimentation may be required. A blood gas would likely be required.
Supplementary oxygen therapy
Nasual cannula- long tube and nasal prongs. Promotes ability to eat and drink. can only provide up to 4L of oxygen delivery
Simple semi-rigid plastic mask- this is limited to a maximum amount of deliver between 5-10L/min
Venturi barrels/ Venturi masks-come in a variety of colours that are associated with oxygen % delivered they fit onto specific face masks:
- 24% blue
- 28% white
- 35% yellow
- 40% red
- 60% green
Tracheostomy masks- as specially designed to fir on a tracheostomy.
Non-rebreathe mask with reservoir- these masks will deliver between 60-90% oxygen when delivered appropriatley using 10-15L/min. The bag is inflated, then the patient can inhale safely, and the valve will prevent expired air flowing back in the mask chamber.
Normal/abnormal ranges
Breathing/respirations:
- Adults 12-18 breaths/min
- Children anything beteen 12 to 50 breaths/min
- The respiratiry rate is usually the first indicator for the patient in distress
Oxygen
- The british thoracic societ (BTS) advised that oxygen (o2) levels should be 94%-98% in patients without oxygen affection conditions like COPD
- BTS advise that those who have a diagnosis of COPD should aim for oxygen levels between 88%-92% on air.
- N.B: someone with COPD may also have levels of oxygen on air that are higher than 92%. This is ok. The issue comes with providing additional oxygen
Breathing terminology
- Bradypnoea- slow respiratory rate
- Tachypnoea- fast respiratory rate
- Apnoea- Brief episode of absent breathing (sleep apnoea)
- Dyspnoea- difficulty in breathing
- Hyperventilation- fast breathing
- Hypoventiltion- slow breathing and sometimes irregular in nature
- Hypoxia- low levels of oxygen
- Hypercardia- high levels of carbon dioxide
- SPO2- Levels of peripheral arterial oxygen
- SAO2- the result of oxygen within arterial blood
- PaCO2- the result of carbon dioxide in arterial blood
Consciousness and blood glucose
The neurological examination will tell you about the patients central nervous system functionality. The central nervous system (CNS) is the brain and the spinal cord.
The nervous system is probably the most complex of all the body systems. The 3 basic functions include:
- sensory- information carried to the brain via the spinal cord and cranial nerves
- Integrative- this is simply information interpretation and response
- Motor response- the body responds by activationg muscles and glands through cranial and spinal nerves
Consciousness is the wakefulness or awareness of surroundings. So a conscious patient will be aware of sensory information e.g. touching and sound
Using the ACVPU is a quick way of assessing the neurological status of a patient. Another screening tool we can use in practice is assess the neurological status of a patient is the Glasgow coma scale (GCS)
- A- alert
- C- confusion
- V- voice
- P- pain
- U- unresponsive
Neurological status
The neurological status of the patient is important because subtle changes can happen for a variety of reasons
Disease of the brainstem:
- Brainstem stroke- haemorrhagic or infarct
- Chronic alcholism- wernicke- korsakoff's syndrome
- Multiple sclerosis
Pressure on the brainstem
- Tumors
- cerebral stroke that is usually haemorrhagic
Diffuse brain dysfuntion
- Drugs
- Epilepsy
- Sepsis
- Alteted electrolytes
- Diffuse brain injury from trauma
- Liver failure and Respiratory failure
ACVPU
A- alert and talking
C- new confusion (the person was not confused before assessment)
V- responds to voice
P- only responds when to pain or stimulated pain
U- unresponsive
a person who is not alert is considered to have an altered level of consciousness and is assessed using the above ACVPU
Capillary blood glucose
Monitoring the blood glucose provides information on how the body is controlling the glucose for metabolism.
In patients who inject insulin, blood glucose monitoring is essential.
Blood glucose is measured in mmol (millimoles per litre) and the normal ranges are between:
- under 18 years= 4-8 mmol premeal and less then 10 mmol post meal
- over 18 years= 4-7 mmol premeal and less than 9 mmol post meal
Capillary blood glucose monitoring is a good procedure for those with an altered level of consciousness as a potential reason for an altered level of consciousness. e.g. both hypoglycemia (low blood glucose) and hyperclycemia (high blood sugar) can alter the neurological status. Someone can appear slurred in speech or drunk.
All children should have a capillary blood glucose measured as part of the assessment, there is a specific place on the PEWS chart for this
Emergency care
The patient who has an altered level of consciousness maybe at risk of losing their airway and develop respiratory and cardiovascular complications
Temperature
Body temperature represents the balance between heat production (metabolism) and heat loss (respirations).
The control center for thermoregulation is the hypothalamus and receives signals from skin receptors and organs. The hypothalamus has neurons in the anterior and posterior portion called the preoptic area hich acts as a thermostat.
Thermoregulation is a metabolic reaction- if the body temperature is raised, it is because the metabolism of the person is faster than it should be, and there is a sudden increase on our tissues demand for fuel, such as: oxygen and glucose.
Our body has different temperatures. Core body temperature is found in blood-supplying organs (brain) as well as in the thoracic cavity and our abdominal cavity. Our skin and peripheries tends to have lower temperature.
The body attempts to maintain its own heat with responses like vasoconstriction, vasodilation and sweat glands
What can affect temperature
- Medications
- Environmental exposure
- Circadian rhythms- time of day
- Shift patterns
- Ovulation
- Extremes of age- Young people probably shiver at a temperature of 36 degreed celsius, whereas someone musch older may npt shiver until a temperature is much lower. In newborns our low birth children thermoregulation is inadequate, and older people tend to have a lower body temperature.
- Some conditions may cause a person to not feel hot or cold. Hypoglycaemia and adrenal insufficiency.
- During surgery when internal organs are exposed as well as the use of drugs that may inhibit vasoconstriction
What can affect temperature
- Medications
- Environmental exposure
- Circadian rhythms- time of day
- Shift patterns
- Ovulation
- Extremes of age- Young people probably shiver at a temperature of 36 degreed celsius, whereas someone musch older may npt shiver until a temperature is much lower. In newborns our low birth children thermoregulation is inadequate, and older people tend to have a lower body temperature.
- Some conditions may cause a person to not feel hot or cold. Hypoglycaemia and adrenal insufficiency.
- During surgery when internal organs are exposed as well as the use of drugs that may inhibit vasoconstriction
How to measure temp
- Tympanic- in the ear canal with an electronic device
- Oral- using the heat pockets whic are sublingual pockets of tissues at the base of the tougue (less commonly used due to accuracy and safety)
- Temporal- The temples on the side of the head
- Axilla- Under the arm (this is used in children but can be used in adults)
- Rectally- readings tend to be higher, but obviously due to the nature, it is less used. There are contraindications for its use too
Temperature is an indicator for internal cellular distress, for example in sepsis temperature is a key aspect of the assessement.
In trauma, hypothermia must be prevented as this can contribute to a life-threatening condition
What are the normal temp ranges
- Adult normal ranges are from 36- 37.5 degrees celsius
- Child normal ranges are from 36.6- 37.7 degrees celcius
- Children can also have "febrile convulsions" which are seizures like states that can occur because of very high temperatures
- N.B- Temperature change should be documented on the NEW2/PEWS chart and let the nurse know immediately.
Temperature terminology
Hypothermia- this is when the body's temperature is below 35 degrees, oral thermometers can fail to give a true reading.
- 3 stages of hypothermia, mild, moderate or severe.
- 3 Known entities of hypothermia: induced, endogenous and accidental
Pyrexia- is associated with a significant temperature above 37.6 degrees. This can occur for a variety of reasons including a reaction to blood transfusions
Hyperthermia- This is related to the bodies thermoregulation being overwhelmed and usually indicates an infection. However, some life threatening conditions that are not infection related may cause this response in a person. Other conditions include damage to the hypothalamus for example in a traumatic injury.
Hyperexia- Is when the body temperature exceeds 40 degrees celsius.
Apyrexia- the body is at its normal body temperature
Febrile- the body is showing signs of fever
Related discussions on The Student Room
- 5 careers for Adult Nursing Graduates »
- Nursing Placements at City University of London »
- Midwifery »
- Nursing placement »
- Nursing at City university of London »
- LSBU BSc Mental Health Nursing 2024 »
- What things should I know for a nursing interview? »
- Official University of Roehampton Offer Holders Thread for 2024 entry »
- Day in a Life of a Third Year Student Nurse »
- Child nursing - placement hours »

Comments
No comments have yet been made