Hydration
- Created by: Charlotte170289
- Created on: 10-01-21 15:41
Fluid compartments
Intracellular fluid (ICF)- The composition of Intracellular fluid is largely controlled by the cell itself because there are selective uptake and discharge mechanisms present in the cell membrane. The body consists of around 70% intracellular fluid. Intracellular fluid contains water and disolved solutes and proteins. The solutes are electrolytes, which help keep out body functioning properly. An electolyte is an element or compound that, when dissolved in fluid, breaks up into ions. There are a lot of electrolytes inside the cell, but potassium, magnesium and phosphate have the greatest concentration.
Extracellular fluid (ECF)- consists mainly of blood, plasma, lymph, cerebrospinal fluid and fluid in the interstitial spaces of the body. Other extracellular fluid are present in very small amounts: their role in lubrication. These extracellular fluids contain ions and nutrients which require the cell.
Extracellular fluid id divided into 2 types:
- An extravascular compartment or Interstitial fluid
- Intracascular compartment or blood volume
Body water = 60% of a patients body weight.
Body fluid percentage
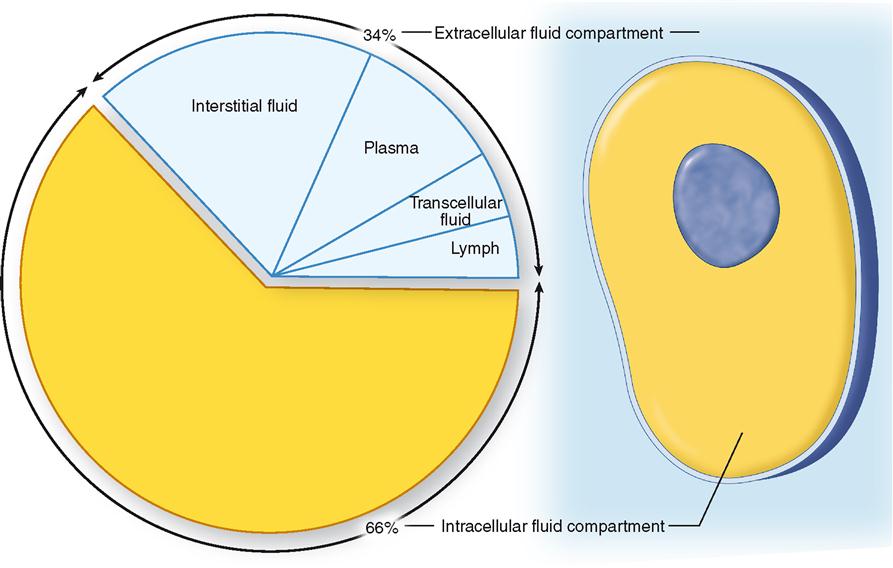
ICF and ECF %
- ICF makes up 66.66%
- ECF makes up 33.33%
ECF Fluids outside the cell
- 80% Interstitial fluid
- 20% plasma
Glossary
- Solute- the substance that dissolved
- Solvent- substances in which solute is dissolved
- Osmolality- concentration of solute per Kg of water
- Osmolarity- concentration of solute per L of solution
- Substance- substance that dissolve in other substances
Composition of the body fluids
The fluids circulating throughout the body in the ECF and ICF spaces contain:
Electrolytes- an ionic compound e.g. sodium chloride, dissolved in water is called an electrolyte because it conduts electricity. Electrolytes are important in the body constituents because they: conduct electricity, essential for muscle and nerve function, exert osmotic pressure, keeping body fluids in their own compartment, act as a buffers to resist pH changes in body fluids.
Minerals- Essential minerals are sometimes divided up into major minerals (macrominerals) and trace minerals (microminerals). These two groups of minerals are equally important, but trace minerals are needed in smaller amounts than major minerals. The amounts needed in the body are not an indication of their importance. A balanced diet usually provides all of the essential minerals e.g. sodium, potassium, calcium
Cells- Cells are the basic building blocks of all animals and plants. Inside cells are various structures that are specialised to carry out a particular function. Both animal and plant cells have these components: Cell membrane – this surrounds the cell and allows nutrients to enter and waste to leave it. Nucleus – this controls what happens in the cell. It contains DNA, the genetic information that cells need to grow and reproduce. Cytoplasm – this is a jelly-like substance in which chemical reactions happen. Mitochondria – these are the powerhouse of the cell. They are structures where respiration takes place.
Movement of the body fluids
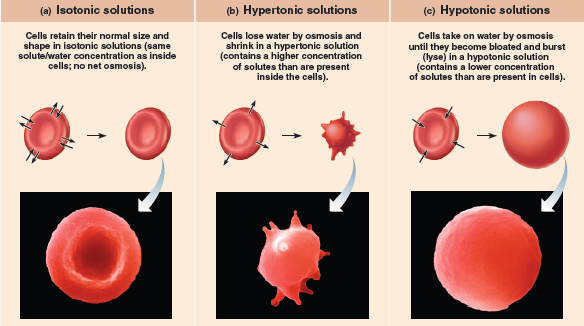
Diffusion- The movement of ions and molecules from and area of high concentration to an area of low concentration in an attempt to acheive an isotonic balance.
Osmosis-The movement of water across a semipermeable membrane from a dilute/hypotonic solution (with low osmotic pressure) to a more concentrated/hypertonic solution (which has a higer osmotic pressure.
Active transport- The movement of solutes (ions and molecules) across a membrance (usually) against a concentration gradient involving the use of energy (ATP) and carrier proteins.
Filtration- The movement of water, ions and molecules from an area of higher pressure to an area of lower pressure, usually across a semipermeable membrane, due to the hydrostatic pressure of the fluid.
Diffusion & Osmosis

Active transport
Isotonic, Hypertonic & Hypotonic
Electrolytes
- A substance that dissociates into ions when dissolved in a solution and attains the ability to conduct electricity.
- Chemically, electrolytes are substances that become ions in solution & acquire the capacity to conduct electricity.
- Essential for normal function of the cells and our organs
- Contains sodium, potassium, chloride and bicarbonate
Sodium (Na+)
- 135 to 145 mEq/L (135-145 mmol/L)
- Major positive ion in fluid found outside the cells
- Regulates the total amount of water in the body and the transmission into and out of the cells.
mmol/l= millimoles per liter
Potassium (K+)
- 3.5 to 5.0 mEq/L (3.5 to 5.0 mmol/L)
- Major positive ion found inside the cells.
- Regulation of the heartbeat and function of the muscles
Chloride (Cl-)
- 98 to 108 mmol/L
- Major anion (negatively changed ion) found outside the cells and in the blood
- Helping the body maintain a normal balance of fluids
Bicarbonate (HCO3-)
- 22 to 33 mmol/L
- Acts a buffer to maintain the normal level of pH in the blood and other fluids in the body/
- Measured to monitor the acidity of the blood and body fluids
Third spacing
- Occurs when the fluid is "trapped" in the interstitial space
- Fluids shifts from the vascular space into an area where it is not readily accessible as extracellular fluid
- This fluid remains in the body but is essentially unavailable for use, causing an isotonic fluid volume deficit
- Patient may not menifest fluid loss or weight loss
Causes of fluid shifts
- Albumin (the main plasma protein which generates plasma colloidal osmotic pressure and served as a transport protein) losses can occur in liver failure, liver dysfunction and malnutrition
- Albumin losses can lead to fluid shifting into the peritoneum, causing ascities (accumulation of fluid in the peritoneal cavity)
- Destruction of endothelial cells, such as in bowel surgery, can cause fluid to move and be trapped in the interstitial space
- Fluid trapped in the lungs can lead to pulmonary edema.
Inside the cell
- Interstitial fluid trapped can cause compression of the microvascular, resulting in hypoperfusion and ischemia.
- Inflammatory "mediators" are released into the bloodstream, which can lead to systemic inflammatory response syndrome (SIRS)
- Multiple organ dysfunction syndrome (MODS) occurs, leading to organ failure and death.
What happens when fluid shifts
- With ecreased circulating volume, baroreceptors (sensory receptors that respond to changes in pressure) in the aorta are activated
- Sympatheric nervous system releases epinephrine (adrenaline) and norepinephrine (hormone that is released by the adrenal medulla), causing vasoconstriction and an increased heart rate.
- Kidneys launch the renin-angiotensin-aldosterone system ( is a hormone system within the body that is essential for the regulation of blood pressure and fluid balance) in response to a lower glomerular filtration rate (how the kidneys clean the blood)
- All this happens with the goal of increasing circulating volume, blood pressure and cardiac output
Fluid shift in the bowel
- Causes abdominal distention
- Measure bladder pressure and abdominal girth at least every 4 to 8 hours while signs are abnormal
Monitoring the patient
- Fluid shift will either resolve over the next several hours (up to 48 hours) or the patient will continue to develop bowel edema and eventually ischemia (a reduction in blood supply to tissue that results in the supply being insufficient)
- Closely monitor vital signs, urine output, peripheral perfusion (bloody supply to peripheral's toes, fingers) mental status, ventilation/perfusion status, hematocrit/hemoglobin, serum electrolytes (elevated lactate may indicate bowel ischemia)
Fluid Resuscitation
- Administer maintenance I.V. isotonic fluid plus intermittent colloids (i.e. albumin) pulls fluid from the interstitial spaces into the intravascular space
- Small dose of a loop diuretic (diuretic that work by inhibiting the sodium-potassium-chloride and co-transporter in the thick ascending loop of Henle, located in the kidneys) such as furosemide (Lasix) may be ordered if the kidneys cant get rid of excess fluid.
- If hemoglobin is low, infuse blood products such as packed red blood cells, as ordered to help increase oxygen and pull fluid from the interstitial space.
Oedema
- In fluid volume excess, both intracascular and interstitial spaces have an increased water and Na (sodium) content.
- Excess interstitial fluid (space within a tissue or organ)
- Most apparent areas where the tissue pressure is low like around the eye
- Dependent tissues known as dependent oedema, where hydrostatic capillary pressure is high.
3 main mechanism of oedema
- Increase capillary hydrostatic pressure ( the pressure exerted by the blood against the artery wall by the heart pumping blood at force)
- Decrease plasma oncotic pressure (a form of osmotic pressure induced by proteins, notably albumin, in a blood vessel's plasma (blood/liquid) that displaces water molecules)
- Increase capillary permeability (movement of blood plasma in and out of the capillaries)
- (osmotic pressure is the pressure exerted by plasma proteins and some electrolytes in the plasma inside the capillaries, pulling water and small molecules towards them)
Pitting Oedema
- That leaves a small depression or pit after finger pressure is applied to the swollen area.
- The pit is caused by movement of fluid to adjacent tissue, away from the point of pressure
- Within 10 to 30 seconds the pit normally disappears.
Related discussions on The Student Room
- Top Tips from our Nursing Students »
- Nursing Dissertation Ideas. »
- Adult nursing vs child nursing »
- Adult or child nursing? »
- which course to apply for first »
- Mental health nursing »
- Adult Nursing Placements »
- Adult or children nursing degree »
- Midwifery Applicant 2024 (Urgent) »
- Nursing degree Nottingham Trent university »
Comments
No comments have yet been made