The urinary system
- Created by: Charlotte170289
- Created on: 11-01-21 10:01
Urinary system

Urinary systems functions
The urinary system plays a vital part in maintaining homeostasis of water and electrolytes within the body.
- Conserves nutrients
- Eliminates organic waste
- Regulates plasma ion levels
- Regulates blood volume and blood pressure- adjusts water loss, releases cardiovascular hormones
- Stabilizes blood pH
Main components
- Kidneys
- Ureters
- Urinary bladder
- Urethra
The kidneys
The kidneys produce urine, which contains metabolic waste products including the nitrogenous compounds urea and uric acid, excess ions and sometimes excrete drugs.
The main functions of the kidneys are:
- formation of urine, maintaining water, electrolyte and acid-base balance
- excretion of waste products
- Production and secretion of erthropoietin, the hormone that stimunates formation of red blood cells (erythropoiesis)
- Production and secretion of renin, an important enzyme in the long term control of blood pressure.
The kidneys lie on the posterior abdominal wall, one on each side of the vertebral column. The kidneys are retroperitoneal (sit in the cavity behind peritoneal abdominal cavity) The left kidney is superior to the right one (due to the presents of the liver). The kidneys have a sheath of fibrous connective tissue, the renal fascia that encloses the kidney and the renal fat. They also have the Renal artery and renal vein which make them very vascular organs
Kidney location (back view)

The kidneys
The kidneys have 2 main parts of internal anatomy:
- Nephrons (functional unit)- is a tubule that is closed at one end and opens into a collecting duct at the other end. Contains around 1.2 million functional units per kidney. The nephrons produce urine. The nephrons are also described into 3 parts- the proximal convoluted tubule, the medullary loop (loop of henle) and the distal convoluted tubule, leading into a collecting duct.
- Renal pelvis: urine collects here from calyces, urine leaves renal pelvis to the ureter.
Kidneys

The kidneys- what they do
The nephrons are the besic functional unit of the kidney.
The kidneys form urine, which passes to the bladder for storage prior to excretion. The composition of urine reflects the exchange of substances between the nephron and the blood in the renal capillaries. Waste products of protein metabolism are excreted, water and electrolytes levels are controlled and pH (acid-case balance) is maintained by excretion of hydrogen ions.
There are 3 processes involved in the formation of urine:
Filtration- takes place thought the semipermeable ealls of the glomerulus and glomerular capsule. Water and other small molecules readily pass through, although some are reabsorbed later. The fluid filtered from the bloodstream into the glomerular capsule is now called filtrate, and its composition well be adjusted as it passes through the other parts of the renal tubule. Blood cells, plasma proteins and other large molecules are too lattge to filter through and remain in the capillaries.
Selective reabsorption- Most reabsorption from the filtrate back into the blood takes place in the proximal convoluted tubule. Many substances are reabsorbed here including water, electrolytes and organic nutrients such as glucose, amino acids. Only 60-70% of filtrate reaches the medullary loop, much of this especially water, sodium and chloride are reabsorbed into the loop. Around 99% of what is filtered from filtration is reabsorbed i.e. calcium, sodium and potassium
Secretion- The remaining waste products (via the ureters into the bladder)
This process results in urine formation
To summarise
The kidneys remove waste products from the blood: they also assist in the regulation of blood volume, and blood pressure, ion levels and blood pH
Nephrons are the primary functional units of the kidneys with 3 main functions
Resulting in producting urine
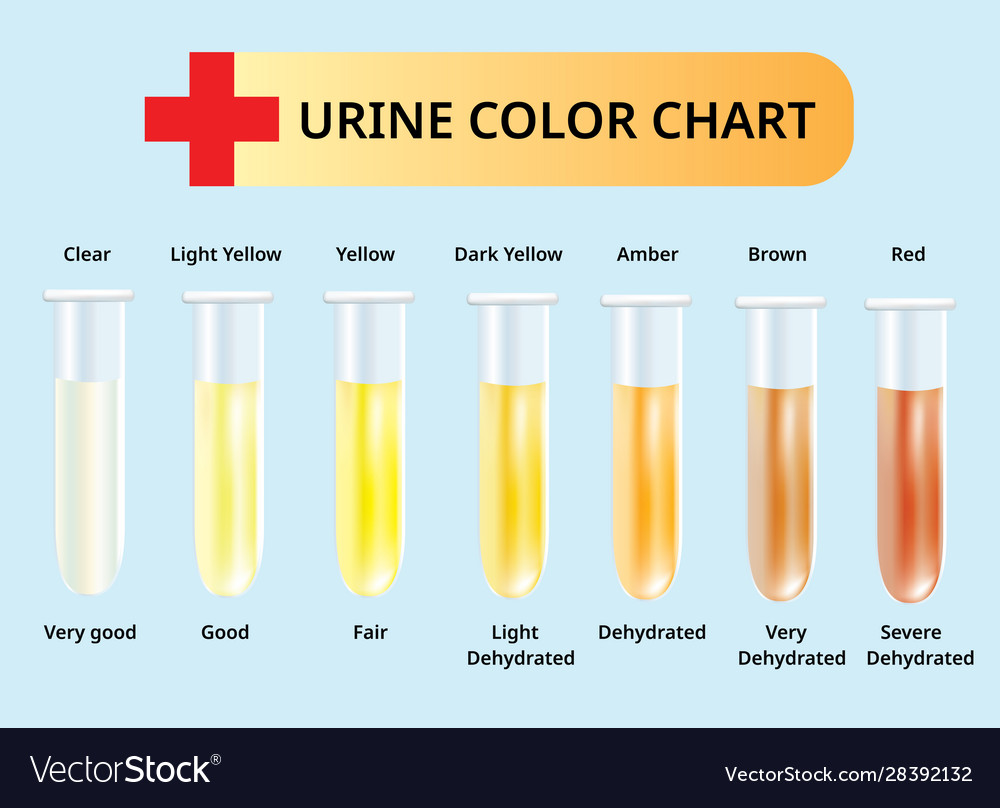
Composition of urine
Urine is clear and amber in colour due to the presence of the pigmented substance uronilin. This is generated following haemolysis when some of the urobilinogen produced in the kidneys is converted to urobilin. The specific gravity is between 1020 and 1030, and the pH is around 6 (normal range 4.5 - 8). A healthy adult passes from 1000 to 1500 mL per day. The volume of urine produced and the specific gravity vary, according to fluid intake and the amount of solute excreted. The constitutents of urine are:
- Water 93-97%
- Urea 2%
- Uric acid
- creatinine
- ammonia
- sodium
- potassium
- chlorides
- phosphates
- sulphates
- oxalates
What should urine look like
- The normal output produced by a healthy adult or child should be between 800ml-2000ml in 24 hours
- The obviously can vary per patient for various reasons
- Hourly urine output is calculated as follows 0.5ml/kg/hr
Fluid management
Input vs output
Pyrexia (high temperature), Diarrhoea and vomiting, being a child

After urine production
Urine modification ends when fluid enters the renal pelvis (in the kidney)
It needs transporting, storing and excreting using the following:
- 2 ureters (if 2 kidneys)
- Urinary bladder
- Urethra
Transport, storage & excretion
- Ureters- carry urine from the kidneys to the urinary bladder. They are hollow muscular tubes about 20-30cm long with a diameter of approximarely 3mm. The ureters is continuous with the funnel shaped renal pelvis. It travels downwards through the andominal cavity, behing the peritoneum in front of the psoas muscle into the pelvic cavity, and passes obliquley through the posterior wall of the bladder. Peristalsis pushes urine towards the bladder via peristaltic waves, increasting in frequency with the volume of urine produced and sending little amounts of urine along the ureter towards the bladder.
- Urinary bladder- the bladder opens into the urethra at its lowest point, the neck. The bladder is composed of three layers: the outer layer of loose connective tissue containing blood and lymphatic vessels and nerves, covered in the upper surface by the peritoneum. The middle layer, consisting of interlacing smooth muscle fibres and elastic tissue loosely arranged in three layers. This is called the detrusor muscle, and when it contracts it empties the bladder. The inner mucosa, composed of transitional epithelium that readily permits distension of the bladder as it fills. (muscular sac for urine storage, contraction forces urine into the urethra)
- Urethra- is a canal extending from the neck of the bladder to the exterior, at the external urethral orifice. The striated muscle forms the external urethral sphincter and is under voluntary control. The mucosa is supported by loose fibroelastic connective tissue containing blood vessels and nerves. Urethral sphincter has 2 muscles (internal/external) which is used to control the exit of urine when they contract the urethra is closed. Crucial for maintenance of urinary continence.
Male urinary bladder

How we excrete urine
- Micturition reflex- This stimulates involuntary contraction of the detrusor muscle and relaxation of the internal urethral sphincter, and expesl urine from the bladder: this is known as micturation, urination or voiding of urine. When the bladder control is established the micturition reflex is still stimulated but sensory impulses also pass upwards to the brain and there is awareness of the need to pass urine as the bladder fills. Initiated by stretch receptors in the bladder walls.
- Voluntary urination involves reflex plus relaxation of external urethral sphincter.
- Internal urethral sphincter opens
- Complex neurological links between bladder, spinal cord and brain stem.
- Many reasons why this doesnt happen correctly, or happens involuntary i.e. neurological disorders, trauma, surgery, malformation etc. Resulting is incontinence
The importance of managing incontinence
- Its distressing, unpleasant and socially disruptive for patients.
- Clinical reasons i.e. post surgery to promote healing, measure output in acutely unwell.
- Prevent other related issues developing such as skin breakdown
- Remember holistic, individualised care is key therefore thorough assessment is required.
Managing continence
Moisture associated skin damage
Moisure associated skin damage (MASD)
}Irritation and breakdown of the skin }Over exposure to moisture/chemicals in urine }Increased risk of bacterial growth/infection }Increasing risk for pressure damage/moisture lesions Inflamation of the skin with or without erosionUrinary catheter
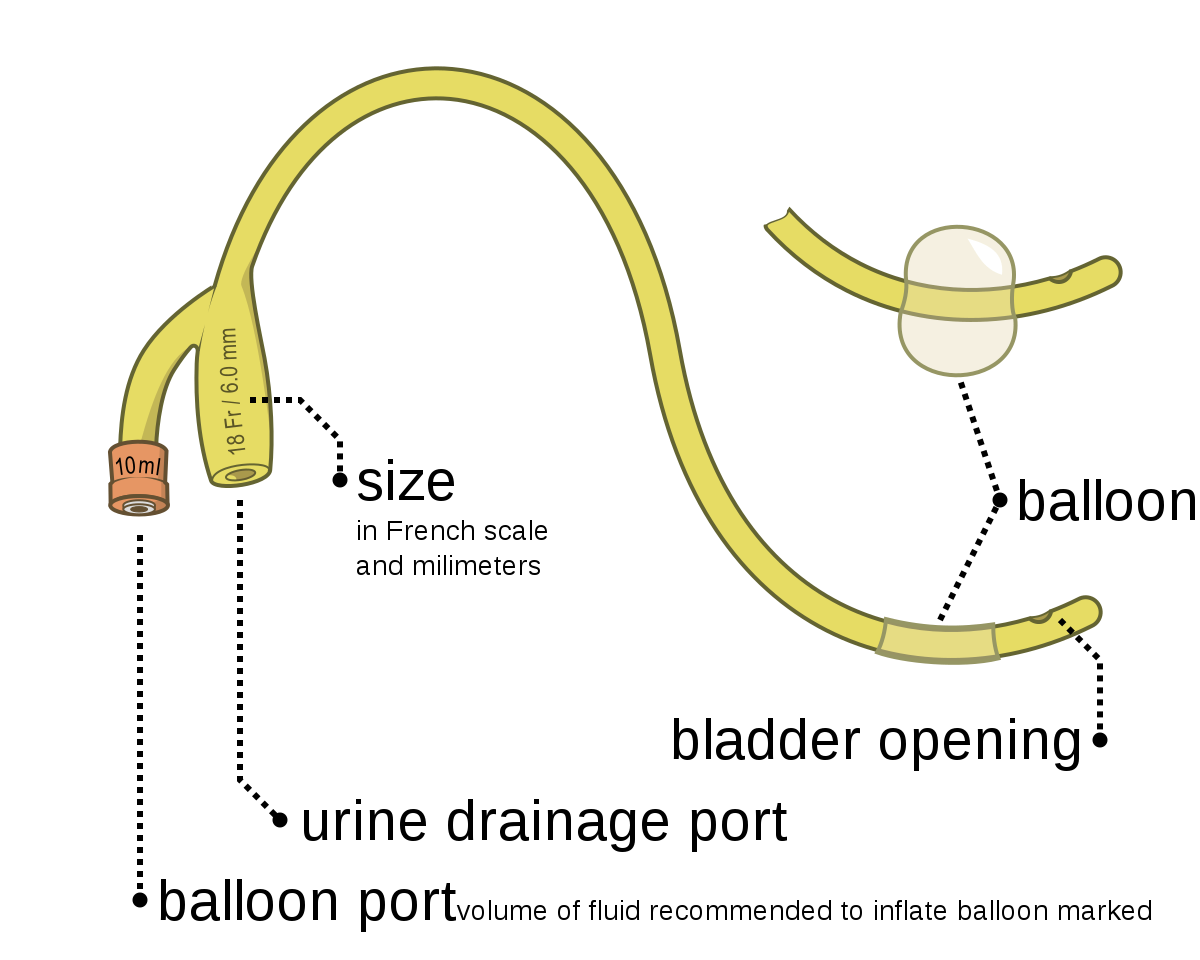
Catheter specimen of urine
Urinalysis
Urinary system in perspective
- Integumentry system- Sweat glands assist in elimination of water and solutes, especially sodium and chloride ions: Keratinized epidermis prevents excessive fluid loss through the skin surface: epidermis produces vitamin D important for the renal production of calcitriol.
- Skeletal system- Axial skeleton provides some protection fro kidneys and ureters: pelvis protects urinary bladder and proxiaml portion of urethra. Conserves calcium and phosphate needed for bone growth.
- Muscular system- Sphincter controls urination by closing urethral opening: muscle layers of truck provide some protection for urinary organs. Removed waste products of protein metabolism, assists in regulations of calcium and phosphate concentrations.
- Endocrine system- Aldosterone and ADH adjust rates of fluid and electrolyte reabsorption in kidneys. Kidney cells releases renin when local blood pressure declines and erythropoietin (EPO) when renal oxygen levels decline.
- Cardiovascular system- Delivers blood to capillaries, where filtration occurs, accepts fluids and solutes reabsorbed during urine production. Releases renin to elevate blood pressure and erythropoietin to accelerate red blood cell production
- Lymphatic system- Provides specific defenses against urinary tract infections. Eliminates toxins and wastes generated by cellular activities: acid pH of urine provides nonspecific defense against urinary tarct infections.
Urinary system in perspective
- Respiratory system- Assists in the regulation of pH by eliminating carbon dioxide. Assists in the elimination of carbon dioxide: provides bicarbonate buffers that assist in pH regulations
- Digestive system- Absorbs water needed to excrete waste at kidneys: absorbs ions needed to maintain normal body fluid concentration: liver removes bilirubin. Excretes toxins absorbed by the digestive epithelium: excretes bilirubin and nitrigenous wastes produced by the liver: calcitrol production by kidneys aids calcium and phosphate absorption along the digestive tract
- Reproductive system- Accessory organ secretions may have antibacterial action that helps prevent urethral infections in males. Urethra is males carries semen to the exterior


Comments
No comments have yet been made