Wound management (SSKIN)
- Created by: Charlotte170289
- Created on: 07-01-21 14:49
Cost to the NHS/ Patients
NHS
- The total cost to the NHS in the UK to treat pressure ulcers is estimated to be £1.4-£2.2 billion annually. 90% of this is healthcare professionals time, 10% on treatment/ specialist equipment.
- 7 million patients affected by pressure ulcers
- Extended length of stay in hospital
- Increase in need from aging and growing population
The patient
- Can be life threatening
- Can lead to severe disabilities/ amputation
- Infection and osteomyelitis
- Extended hospital stay
- The need for surgery or prolonged immobility
- Along with exudate and leaking dressings, possible malodour and embarrassment but most importantly pain and suffering
Definition of pressure ulcers
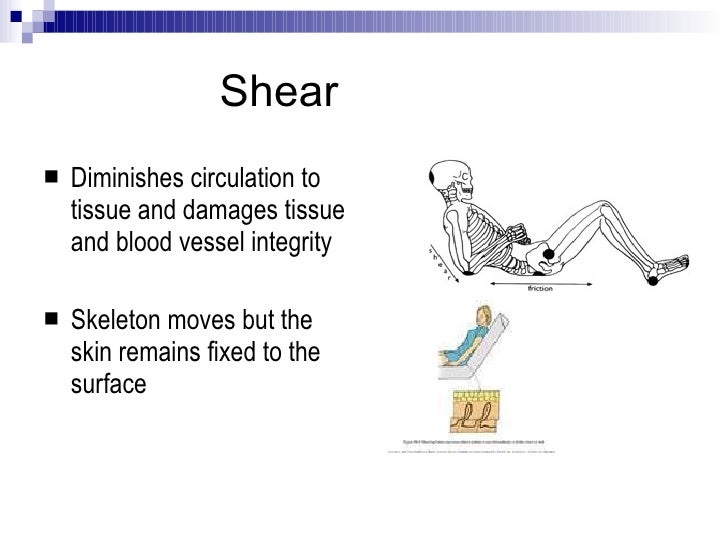
A pressure ulcer is a localised injury to the skin and/or underlying tissue, usually over a bony prominence, as a result of pressure, or pressure in combination with shear.
Prevention is key
As a nurse we need to...
- Identify people at risk of skin breakdown
- Help off load or reduce pressure, shear and friction forces on areas of the skin (SSKIN bundles help)
- Keep skin healthy when patients are in our care
- Be aware how a medical device can cause skin damage especially in children
Risk factors for pressure ulcers
- Extremes of age (that is being very young or the very old)
- Not being able/ willing to move about
- Gender
- Loss of sensation to the skin
- Experiencing urinary or faecal incontinence
Waterlow assessment tool
All risk factors apart (from gender). In some risk assessment tools, being female is scored as a greater risk (Waterlow includes this as a risk)
The Waterlow pressure ulcer risk assessment/prevention policy tool is, by far, the most frequently used system in the U.K. and it is also the most easily understood and used by nurses dealing directly with patient/clients. Intended for use by nurses, healthcare professionals and carers at the patient/client interface.
It must be remembered that "Waterlow", like all risk assessment scoring systems is a simplistic tool.
Professional judgement must be used in determining the risk status of the patient/client.
All assessments and, just as importantly, reassessments must be documented and the plan of care adjusted as necessary.
Pressure ulcer risk assessment
Risk factors are oftern combined within pressure ulcer risk assessment tools but the tools are only as god as the person using them.
They should be used as an aid to decision making and should not be solely relied upon when considering risk.
Examples include:
Waterlow risk assessment tool
Pressure ulcer risk assessment
Risk factors are oftern combined within pressure ulcer risk assessment tools but the tools are only as god as the person using them.
They should be used as an aid to decision making and should not be solely relied upon when considering risk.
Examples include:
Waterlow risk assessment tool
S.S.K.I.N bundles

Prevention
European pressure ulcer advisory panel (EPUAP) identifies:
Strong evidence for:
- use a pH balanced skin cleanser e.g. Dermol
- Develop and implement an individualised continence management plan
- Cleanse skin promptly following episodes of incontinence
Some evidence for:
- Do not massage or vigorously rub skin at risk of pressure ulcers
- Protect skin from excessive exposure to moisture with a barrier product e.g. Cavilon
- Consider a moisturiser to hydrate dry skin
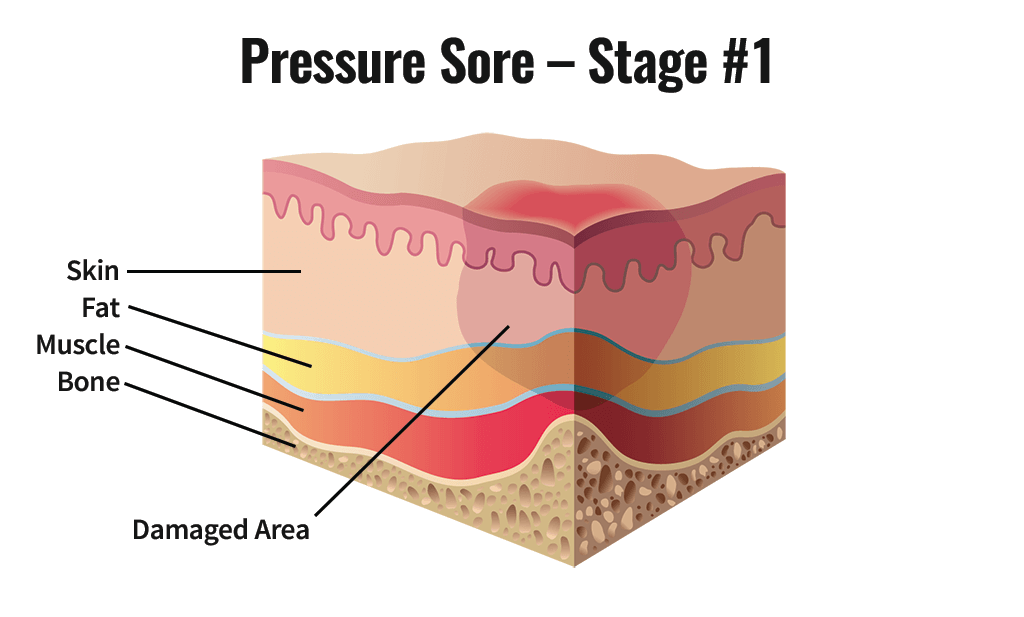
Grade/stage/category 1
Persistent redness
- Non-blanchable erythema (redness) of intact skin.
- Discolouration of the skin, warmth, oedema or hardness may also be used as indicators, particularly on people with darker skin.
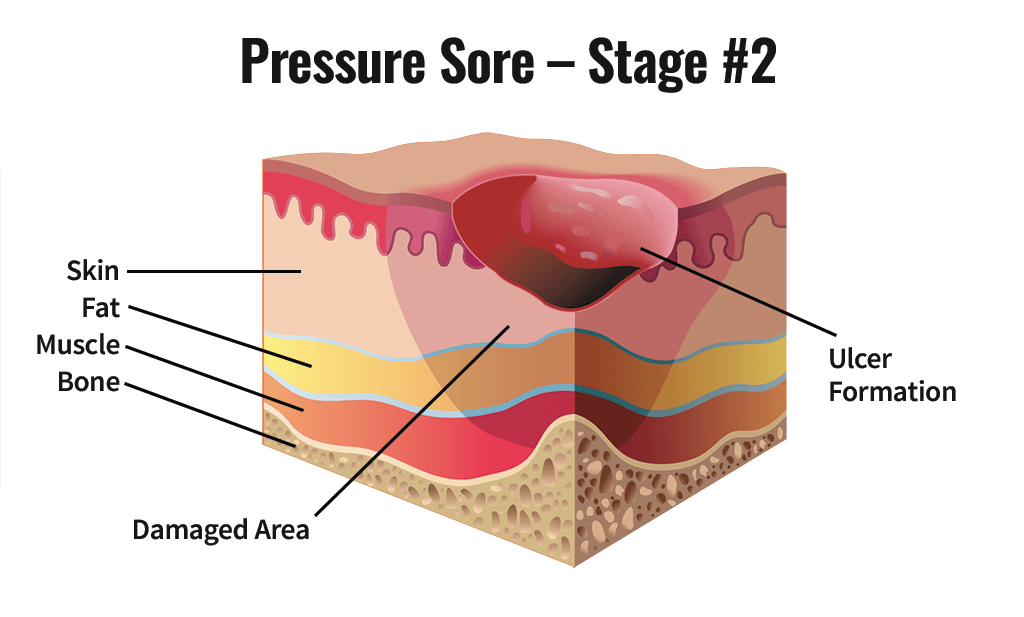
Grade/stage/category 2
- Partial thickness skin loss
- Partial thickness skin loss involving epidermis, dermis or both.
- The ulcer is superficial and presents clinically as an abrasion or blister.
- Cost to heal anywhere from £1214
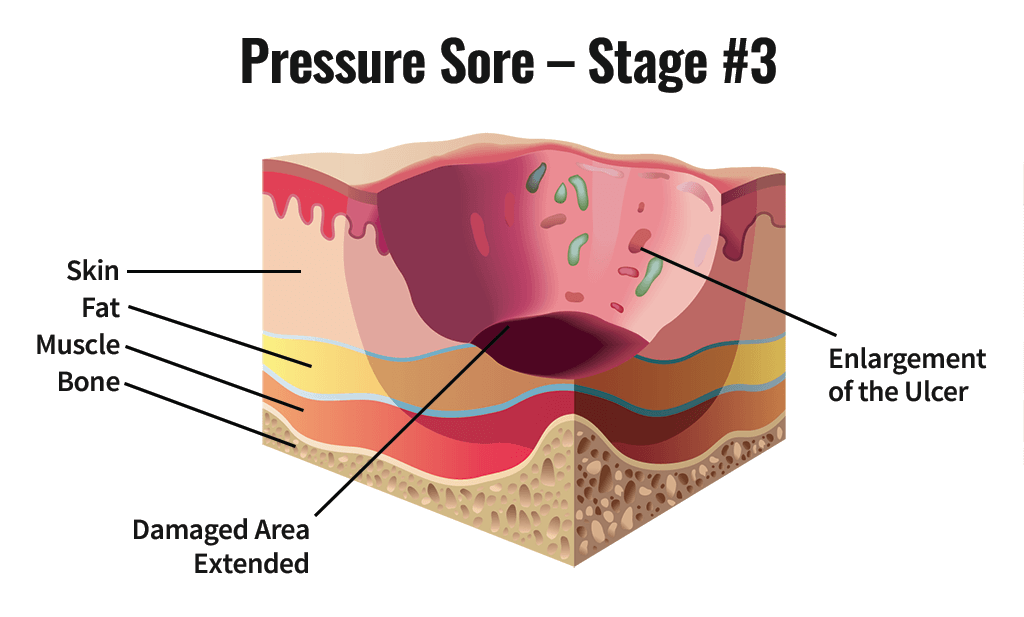
Grade/stage/category 3
- Full thickness skin loss
- Full thickness skin loss involving damage necrosis of subcutaneous tissue that may extend down to, but not through the underlying fascia.
Grade/stage/category 4
- Full thickness tissue loss
- Extensive destruction, tissue necrosis, or damage to muscle, bone, or supporting structures with or without full thickness skin loss.
- Cost to heal roughly £14K

Suspected deep tissue injuries
- Skin changes seen on the surface (coolness, colour changes), are important because they may signal deeper serious injury.
- The tip of the iceberg
- Can also be known as Necrosis or Exchar
Moisture lesion
- A moisture lesion, is one where the skin damage is the result of the skin's exposure to urine and/or faeces or perspiration.
- There are a number of clues which may inducate if the sore skin is caused by moisture and or pressure. These include its location on the body, depth and appearance.
- It is important to know what has caused the sore skin so that the most effective remedy may be put in place.

What is a wound
A wound is defined as a breech in the epidermis or dermis that initiates a process of repair, which can be related to trauma or pathological changes within the skin or the body.
A wound is a breakdown in the protective function of the skin; the loss of continuity of epithelium, with or without loss of underlying connective tissue (i.e. muscle, bone, nerves) following injury to the skin or underlying tissues/ organs caused by surgery, a blow, a cut, chemicals, heat/ cold, friction/ shear force, pressure or as a result of disease, such as leg ulcers or carcinomas.
A wound may also be described in many ways; by its aetiology, anatomical location, by whether it is acute or chronic, by the method of closure, by its presenting symptoms or indeed by the appearance of the predominant tissue types in the wound bed. All definitions serve a critical purpose in the assessment and appropriate management of the wound through to symptom resolution or, if viable, healing.
Wounds Acute or Chronic
Acute wound
- Acute wounds heal in an expected time frame without delay. Examples of an acute wounds are surgical incisions, grazes or an injury such as a laceration. They are most likely to be related to trauma.
- Surgical wounds are incisions made purposefully by a health care professional and are cut precisely, creating clean edges around the wound. Surgical wounds may be closed with stitches, staples or adhesive or left open to heal.
- Traumatic wounds are injuries to the skin and underlying tissue caused by a force of some nature, They are classified by the object that caused the force e.g. Abrasion, puncture, laceration and incision.
Chronic wound
- A chronic wound has delayed healing. Some chronic wounds are present for life. Failure to heal is often related to some underlying disease process such as circulatory disease affecting blood supply to the area. This is a pathological change.
- A chronic wound is a wound that does not heal in an orderly set of stages. Wounds that do not heal within 3 months are considered chronic. For example chronic wounds often remain in the inflammatory phase. These wounds cause patients severe emotional and physical stress as well as creating a significant financial burden on patient and the whole of the health care system. Examples of chronic wounds may be pressure ulcers, diabetic wounds and leg ulcers
Compression treatment
- The internal "problem" that is causing the chronic wound is venous disease.
- Venous blood cannot easily return up the leg due to structural damage to veins.
- Causes skin changes which may result in ulceration

Primary and secondary healing
Primary healing
- This method of healing follows minimal destruction of tissue when the damage edges of a wound are in close apposition.
- Primary wound healing occurs when the tissue surfaces are closed by stitches, staples, skin glue, or steri-strips. A surgical incision that is closed by stitches is a good example. This sort of closure of the wound surfaces creates very little tissue loss, and makes the wound healing process as quick and easy as possible.
Secondary healing
This method of healing follows destruction of a large amount of tissue or when the edges of a wound cannout be brought into apposition e.g. varicose ulcers and pressure ulcers.
Debridement
Debridement is the removal or to un-bride non-living tissue e.g. slough.
Debridement may be done by:
- Dressing selection (a gentle approach)
- Scalpel (clinic/theatre)
- Larvae therapy (maggots)
Dressing selection
When choosing what dressings should be used it is important to:
- Consider carefully what you think has caused the wound
- Decide what your treatment goal is
- Discuss options with the patient, family, carer and child
- Select a dressing or treatment that will help acheive the treatment goal
Remember the treatment goal may not be healing it, but may be more about incleasing well-being.
- Thinking about the patient as well as the wound site is important
- An oftern heard phase in wound management is "treat the whole of the person not the hole in the person"
This phase asks you to think about:
- What the patients views are in respect of treatment of his/her wound
- What other physical, psycho-social or even economic issues do we need to consider in trying to promote healing e.g. alteration of dies to include better quality nutrition, control of diabetes, management of wound related pain.
Ideal dressings
When dressing a wound it is important to remember is the dressing:
- Comfortable, cosmetically pleasing (sight and smell) non-restrictive
- Barrier to infection (imperemable)
- Manages wound fluid
- Doesnt tear or damage the epidermis on removal
- Doesnt traumatise wound bed on removal
- Doesnt cause sensitivity over time
- Thermally insulates
- Doesnt shed particles
- Provides pain relief
- Cost effective (consider wear time issues)
Related discussions on The Student Room
- Nursing placement »
- help with dissertation topic »
- Nursing »
- 5 careers for Adult Nursing Graduates »
- The Difference between Adult Nursing, Child Nursing and Mental Health Nursing »
- Adult or child nursing? »
- Nursing Dissertation Ideas. »
- Adult or children nursing degree »
- Can i go into a university i applied for if i had a unsuccessful interview »
- Nursing degree Nottingham Trent university »


Comments
No comments have yet been made