The Respiratory System
- Created by: rosieevie
- Created on: 20-01-17 17:11
Definitions
- Conducting zone - nose, pharynx, larynx, trachea, bronchi, bronchioles, terminal bronchioles
- Filter, warm and moisten air to conduct it into lungs
- Respiratory zone - O2 and CO2 exchange site within blood
Structure of Respiratory System
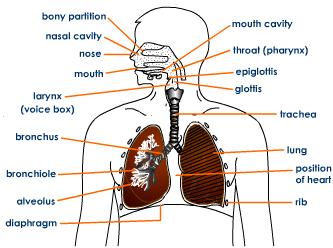
Trachea, Bronchi and Bronchioles
Trachea:
- Cartilagenous rings - hold trachea open + flexible
- Pseudostratified (looks like layers but isn't) ciliated columar epithelium
- Cilia beat towards mouth = mucus swallowed (paralysed by nicotine)
- Goblet cells - create mucus in lumen to trap dust etc
Bronchi:
- Conducting surface and branch repeatedly
- Large in diameter
Bronchioles:
- Smooth muscle and airflow holds airways open
- No fibrocartilengous layer
- Ciliated epithelial cells
- Act as gas exchange site
Thoracic Cavity
- Consists of lungs and diaphragm
- Lungs attached to wall due to interpleural pressure (~4mmHg) = vaccum - lung can move but remain attached
- Drives air movement by volume changes = pressure changes
- Intrapleural pressure always negative - lungs will collaspe otherwise
Lung Compliance
- Relating to lung elasticity
- Decrease - sitffer lung = harder to infalte
- Increase - floppy lung = tissue collapse (especially on exhalation) - emphasema

Alveoli
- Air-filled sacs - expand during inhalation
- Covered with extensive vasculature - gasous exchange
- 3 cell types:
- Type I cell - simple squamous - flat and narrow = thin diffusion pathway
- Type II cell - produce surfactant = detergent which decreases surface tension
- Alveolar macrophages - white blood cell = defence (purify air/immune response)
- Alveolar surface tension - keeps alveolar open and prevents collapse into bigger structures due to pressure difference (surfactanct reduces and equalises pressure)
Cells Lining Airways
Stratified Squamous Epithelial Cells
- Several layers thick = protection
- Withstand abrasion
Ciliated Columnar Epithelial Cells
- Cilia - beat towards mouth so mucus is swallowed
- Paralysed by nictotine
Goblet Cells:
- Secrete mucus - traps dust, bacteria
Alveolar Cells
Inspiration and Expriation
- Expiration - passive stage (2-3s)
- Diaphragm relaxed (dome)
- External intercostal muscles relaxed
- Rib cage in and down
- Decrease in volume - increase in alveolar pressure
- Intrapleural pressure increases
- Inspiration - active stage (1-1.5s)
- Diphragm contracts - downward movement
- External intercostal muscles contract
- Rib cage up and out
- Increases volume - decreases pressure
- Intreapleural pressure decreases
- Quiet breathing - exhalation is passive
Airflow
- Thick pipe - faster airflow
- Increase in diameter increases flow
- Airway diameter regulated by elastic tissues
F ∝ r4
Spirometry Trace Labelled
- Volume - amount of space take up by an object
- Capacity - measure of object's ability to hold a substance
Spirometry Trace Definitions
Residual volume - air remaining in lungs after fully exhaling (keeps lungs open)
Resting tidal volume - air entering lungs at rest (~500ml)
Expiratory reserve volume - maximal volume of air expelled after exhaling
Inspiratory reserve volume - maximal volume of air inhaled during inhalation
Total lung capacity - predicted vital capacity + residual volume
Vital capacity - greatest expelled air volume after taking the deepest possible breath
Functional residual capacity - air remaining in lungs after passive expiration
Measuring Residual Volume
Amount of air left in the lungs after full exhaling (keeps lungs open)
Cannot be measured using conventional spirometry but can be measured by:
- A gas dilution test. A person breathes from a container containing a documented amount of a gas (either 100% oxygen or a certain amount of helium in air). The test measures how the concentration of the gases in the container changes.
- Body plethysmography. This test measures the total amount of air the lungs can hold (total lung volume). For this test, a person sits inside an airtight booth called a plethysmograph and breathes through a mouthpiece while pressure and air flow measurements are collected.
Blood Gaseous Exhange
Oxygen diffuses into blood along partial pressure gradient - changes caused by breathing and circulation.
Warm, humid air in lungs means lower pp in alveoli than atmospheric air
Dalton's Law - in a mixture of gases (air) the total pressure is sum of gas partial pressures
Partial pressure - the pressure a gas would exert if only gas present
At sea level (mostly N2 and O2) - Ptotal = 760mmHg
- N2 = 760mHg x 0.78 = 560mmHg
- O2 = 760mmHg x 0.21 = 160mmHg
Changing altitude = change oxygen's partial pressure
Ventilation and Perfusion
Ventiliation (alveoli) matched to perfusion (pulmonary capillaries) = efficient process
Ventilation = air into alveolus
Perfusion = blood moving past alveoli
Decrease in ventilation (alveolar blockage) -> increase PCO2 and decreases PO2 = blood not oxygenated -> tissue around damaged alvoli constricts arteries, diverting blood to other alveoli
V/Q matching - ratio used to assess efficiency and adaquacy of oxygen from air reaching capillaries
Diffusion Across a Membrane (Fick's Law)
Vgas = (AD/T) x (P1 - P2)
- Vgas = diffusion rate
- A = Area of pathway (directly proportional - large alveolus SA)
- D = gas solubility (directly proportional)
- Limiting factor - reduced by haemoglobin and carbonic anhydrase
- T = pathway thickness (inversly proportional - single squaemous epithelial layer)
- P1 and P2 = pressure differential (directly proportional - high diffusion gradient maintainined by ventilation and circulation)

Red Blood Cells
- Biconcave cells
- Flexible membranes - change shape to pass through narrow capillaries
- Mammalian blood cells - no nucleus (short lifespan - unable to repair and O2 is toxic)
- Bird and reptile blood cells have nuclei
- Haemoglobin - 4 globin proteins w/ 4 haem groups (1 Fe2+ ion = binds to O2)
- 1 RBC can carry 4 O2 molecules
Oxygen-Haemoglobin Dissociation Curve
Oxygen-Haemoglobin Dissociation Curve 2
- S-shaped curve
- Mechanism of O2 unloading
- Unloading cooperatively - made easier by haem shape change
- Right shift (exercise) - lower stauration at same pO2 = more O2 delivered
- High CO2
- Low pH (high H+ conc)
- High tempreature
- High BPG (by-product of glycolysis)
- Left shift (cold) - higher saturation at same pO2 = less O2 delivered
- High pH
- Low temperature
- Blood leaving lungs and entering systemic arteries (arterial blood) - PO2 95mmHg (97%)
- Venous blood returning from peripheral tissues (resting tissue) - PO2 400mmHg (75%)
- Active tissue, heavy exercise (35% saturation) - as low as PO2 15mmHg
- Utilization coefficient - % oxygen haemoglobin gives up to tissues = 25% (exercise <75%)
Myoglobin
- Found in skeletal muscle
- O2 storage/transfer molecule
- 1 subunit - monomeric protein w/ haem ring
- Carries 1 O2 mol - not cooperative
- Dissociation at low pO2
- 20x more myoglobin in whales = able to store O2 at low depths
Carbon Dioxide Transport
- Binds to globin protein of haemoglobin = carbamminoHb (20%
- Dissolves in blood plasma (10%)
- HCO3- in blood plasma (70%)
Carbon dioxide conversion to HCO3-:
RBC facilitate conversion using carbonic anhydrase enzyme:

RBC O2 carrying role not independent of CO2 carrying role = related reactions - removing H+ ions from O2 reaction drives CO2 reaction
Control of Respiratory Activity
Mediated by nervous system - mediators in the brain stem:
- Dorsal respiratory group - inspiraton
- Ventral respiratory group - expiration and inspiraton
- Pneumotaxic center - rate and depth of breathing (smooth it out)
- Apneustic centre - inhibits pneumotaxic centre (controls intensity of breathing)
- Pre-Botzigner complex - controls respiratory rhythm
- Nucleus tractus solitarius - pacemaker
Send outputs to respiratory muscles via respiratory motor pathways
Expiration usually passive process - no need for NS input
Modifying Respiration
- -Higher centers in brian (voluntary) - overidden by simpler centres
- Medullary chemoreceptors - detect changes in pH (CO2 concentration)
- Carotid/aortic body chemoreceptors - detect decreases in CO2 conc
- Hering-Breuer reflex - stretch response in lungs - decrease respiration to prepare for changes in activity - prevents overstretching and damaging muscles
- Proprioceptors - muscles and joints - increase respiration
- Receptors for touch, temperature and pain stimuli
Medullary and Peripheral Chemoreceptors
Medullary Chemoreceptors
- H+ ion concentration (indirectly CO2 levels - cannot cross blood vessel walls)
- In cerebrospinal fluid
- Signals to respiratory control centre - increases respiration
- 5mmHg CO2 increase = x2 respiratory rate
- Chronic exposure to high CO2 levels desensitises them
Peripheral Chemoreceptors
- Detect pO2
- Carotid areas of neck and aortic bodies (arterial blood)
- pO2 drop below 70mmHg to activate (usually 100mmHg)
CO2 prime driver of respiration - 5mmHg increase doubles respiration rate (increase pO2 by 30mmHg before O2 drives)
Real-life Respiratory Situations
Hyperventilating before diving:
- Decrease pCO2 = reduced respiratory urge
- Decreases pO2 = blackout
- Blackout = death
Giving a paitent with COPD O2:
- Paitent has long term pCO2 increase
- Receptors desensitised
- Low pO2 drive
- Giving O2 increases pO2 = lost respiratory drive
- Death - paitent stops breathing
Holding breath until dying:
- Not possible
- Would lose conciousness
- As soon as this occurs breathing would start up again
Related discussions on The Student Room
- Life as a student nurse at Bradford »
- Is the respiratory physiologist qualification recognized in countries where...? »
- pharmacy - struggling with lecture vs textbooks »
- Leeds vs Leicester »
- Suffering from long covid »
- Pharmacy students at uni »
- EPQ suggestions - Pharmacy related »
- What do you actually learn at medical school? »
- question for medical/ healthcare students »
- AQA GCSE Biology Paper 1 (Higher Tier) 2022 »
Comments
No comments have yet been made