A2 OCR Biology, Excretion
- Created by: sophiegoves
- Created on: 19-11-15 09:45
Excretion
Exctetion is the removal of metabolic wast from the body of by products or unwanted substances from normal cell processes.
The main substances to be excreted: Almost any cell product that is formed in excess by chemical processes must be removed, but mainly CO2 from respiration and N2 containing compounds such as urea, produced in liver from excess amino acids.
Where are these substances excreted?
CO2 is passed from the cells of respiring tissues into the bloodstream. It is transported in the blood to the lungs where it can diffuse into the alveoli to be exctreted as we breathe out.
Urea is produced by breaking down excess amino acids in the liver. This porcess is called deamination. The urea is then passed into blood stream to be transported to kidneys. In the kidneys the urea is removed from the blood to become part of urine. Urine is stored inthe bladder before being excreted by the uerthra.
Why removal of CO2 is important
Carbon Dioxide:
- Majority of CO2 is carried in blood a hydrocarbonate ions. This also forms H+ ions. The H+ combine with Hb and compete with O2 for spce. If there is lots of CO2, then there is less oxygen transport by Hb.
- CO2 combines directly with Hb to form carbaminoheamoglobin. This molecule has a lower affinity for oxygen than normal heamoglobin.
- Excess CO2 can cause resporatory acidosis. The CO2 dissolves in blood plasma, and then combines with water to produce carbonic acid.
- The carbonic acid then dissociates to release H+ ions
CO2 + H20 ---> H2CO3 ------> H2CO3 ---> H+ + HCO3-
- The H+ lower pH and make blood more acidic. If small changes in pH, medulla oblongata picks it up and increases HR, but if pH drops below 7.35 it results in sklow of difficult breathing and ca nlead to diseases and conditions that directl affect the lungs. This can cause respiratory acidosis.
Why removal of nitrogenous compounds is important
Nitrogenous compounds:
The body cant store proteins or amino acids, however amino acids almost contain as much energy as carbohydrates so would be a waste to get rid of the whole thing. Instead the amino acids are transported to the liver and the toxic amine group is removed (deamination).
The amino group initally forms the very soluble and highly toxic substance, ammonia. This is converted to a less soluable and toxic substance called urea, which can be transported to the kidneys for excretion.
The remaining keto acid can be used directly in respirtation to releae its energy or it may be converted to a corbohydrate or fat for storage.
Deamination: amino acid + oxygen ---> keto acid + ammonia
Formation of urea: ammonia + carbon dioxide ---> urea + water
2NH3 + CO2 ---> CO(NH2)2 + H2O
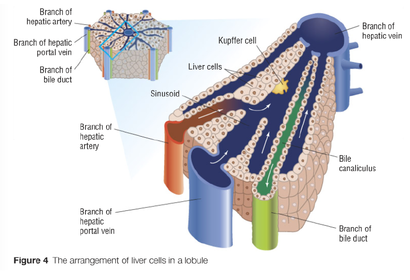
Structure of the liver
The liver cells (hepatocytes) carry out many hundreds of metabolic process and has important role in homeostasis. It is essential that is has good blood supply, so it is arranged to ensure as much blood flows past as many liver cells as possible.
Blood flow to and from the liver: the liver is supplied with blood from 2 sources
- Oxygenated blood from the heart - blood traves from aorta via hepatic artery into liver. This supplies the oxygen that is essential for aerobic respiration. Hepatocytes are very active as they carry out many metabolic processes which require energy so is important there is O2
- Deoxygenated blood from digestive system - this enters the liver via hepatic portal vein, and the blood has high conc of digestive products. The concentrations of compounds will be uncontrolled and the blood may contain toxic compounds that have been absorbed in intestine.
Blood leaves the liver via hepatic vein. This rejoings the vena cava and blood is returned to normal circulation.
A 4th vessel connected to the liver is n ot a blood vessel. It is the bile duct. Bile is secretionm from the liver. It carries bile from the liver to the gall bladder where is is stored until required to aid the digestion of fats in the small intestine.
Structure of liver
Arrangement of cells inside liver
The cells, bloof vessels and chambers inside the liver are arranged so that best possible cotact bwteen blood and hepatocytes. The liver is divided into lobes which are further divided into cylindrical lobules.
As the hepatic artery and hepatic portal vein entre liver they split into smaller vessels. These vessles run between lobules and are called inter-lobule vessels. At intervals, branches from hepatic arter and portal vein entre lobules and the blood from 2 vessels is mixed and passed down a sinusoid. The sinusoid is lined by liver cells.
The sinusoids empty into the intra-obular vessel, a branch of the bepatic vein. The branched of the hepatic vien from different lobules join together to form the hepatic vein which drains blood from liver.
As blood flows along sinusoids it is in close contact with liver cells. They remove and pass molecules in and out of the blood.
One functions of liver cells in to manufacture bile. This is released into bile canaliculi and join togetehr to form the bile duct.
Arrangement of cells inside liver
Liver and Kupffer cells
Liver cells:
Hepatocytes appear to be relatively speciallised. They have a cuboid shape with many microvilli of their surface. However their fuctions include protwin synthesis, transformation and storage of carbohydrates, synthesis of cholesterol and bile salts, detoxification and many other processes. This means that their cytoplasm must be dense and is specialised in the amounts if certain organelles that it contains.
Kuppfer cells:
Kuppfer cells are specialised macrophages. They move about within the sinusoids and are involved with the break down and recycling of old red blood cells. One of the products of heamoglobin breakdown is bilirubin, which is excreted as part of the bile and in faeces. Bilirubin is the brown pigment of faeces.
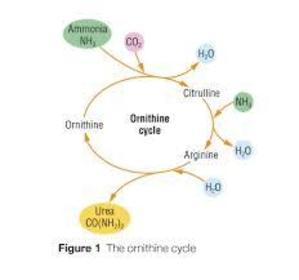
Formation of urea
Each day we need 40-60g of protein however most people eat far more than this. Excess amino acids cant be stored as the amine group makes them toxic but we dont want to waste the energy so it undergoes treatment in the liver before the amino component is excreted. There is two processes, deamination and the ornithine cycle.
amino acid ---(deamination)----> ammonia + keto acid ---(ornithine cycle)---> urea
Deamination: The processof deamination produces ammonia which is soluble and toxic. It must not be allowed to accumulate. It also produces a keto acid which can enter respiration directly.
The ornithine cycle: Ammonia is soluble and toxic so must be converted to less toxic substance quickly. Ammonia is combined with CO2 to produce urea which is less soluble and toxic. This occurs in ornithine cycle. It can then be passed into blood and transported to kidneys, which filters it out to urine.
ammonia + carbon dioxide ---> urea + water
2NH3 + CO2 ---> CO(NH2)2 + H2O
Ornithine cycle
Detoxification
Detoxification is the conversion of toxic molecules to less toxic or non-toxic molecules.
The liver is able to detoxify many compounds. Some compounds are produced inthe body and some are part of out diet (alcohol). Toxins can be made harmless by oxidation, reduction or combinations with other molecules. Liver cells contain many enzymes tha make molecules less toxic. These include catalase, which converts hydrogen peroxide to water and oxygen.
Detoxification of alcohol: Alcohol is a drug that depresses nerve activity. It is broken down by hepatocytes by the action of the enzyme ethanol dyhydrogenase. The resulting compound is ethanal, whis is dehydrogenated further to ethanoate which is combined with coenzyme A which enters respiration. The H+ released in this process are combines with another coenzyme called NAD to form reduced NAD.
ethanol ---> ethanal ---> ethanoic acid ---> acetyl coenzyme A (to respirtation)
NAD breaks down fatty acids in respiration. If liver has to detoxify too much alcohol it has insufficient NAD to deal with the fatty acids, which ocnvert back to lipids are are stored in hepatocytes cause englarged liver called fatty liver. Causes cirrhosis
Structure of kidney
Structure of kidney: Most people have two kidneys. Each kidney is supplied with blood from a renal artery and its drained by the renal vein. The urine passes out of the kidney down the ureter to the bladder where it can be stored before release.
In longitudinal section we can see that thekidney consists of easily identified regions surrounded by a tough capsule. The outer region is the cortex, the inner region is the medula and the centre is the pelvis which leads into the ureter.
The nephron: The bulk of each kidney consists of tiny tubules called nephrons. Each nephron starts in the cortex, where the cappilaried form a knot called the glomerus. This is surrounded by a cup-shaped structure called the Bowman's capsule. Fluid from blood is pushed into the Bowman's capsule by the process of ultrfitration. The capsule leads into nephron which is divided into 4 parts: proximal convoluted tubule, distal convoluted tubule, loop of Henle, collecting duct.
As the fluid moves along the nephron its composition is altered. This is achieved by selective reabsorption. Substances are reabsourbed back into tissue fluid and blood cappilaries surrounding the nephron tubule. The final product in the collecting duct is urine. This passes into the pelvis and down the ureter to the blader.
Structure of kidney
The nephron
Composition change in nephron
- In the proximal convolutued tubule the fluid is altered by the reabsorption if all the sugars, most salts and some wateer.
- In total about 85% of the fluid is reabsorbed here
- In the descending limb of the loop of Henle the water potenital of the fluid is decreased by the addition of salts and the removal of water
- In the acending limb of the loop of Henle the water potential is increased as salts are removed by active transport.
- In the collecting duct the water potential is decresed again by the removal of water. This ensures that the final product (urine) has a low water potential. This means that the urine has a higher concentration of solutes than is found in the blood and tissue fluid.
Formation of urine - Ultrafiltration
Blood flows into the glomerus from the afferent (bring blood into organ) arteriole. This is wider than the efferent arteriole (carries blood away from glomerus). The difference in diameters ensures that the blood in capillaries of the glomerulus us under increased pressure. The pressure in the glomerulus us higher than the pressure in Bowman's capsule. This pressure difference tends to push fluid from the blood into the Bowmans capsule that surrounds the glomerulus.
The barrier betwee the blood in the capillary and the lumen of the Bowmans capsule consists of three layers, the endothelium of capillary, a basement membrane, and the epithelial cells of the Bowmans capsule. They are each adapted to allow ultrafiltraion
- The endothelium of capillaries have narrow gaps between its cells that blood plasma and substances dissolved in it can pass through.
- The basement membrane consists of a fine mesh of collagen fibres and glycoproteins. These act as a filter to prevent passage of molecule bigger than releative molecular mass of 69000. This means most proteins and all blood cells are held in capillaries of glomerulus.
- The epithilial cells of Bowmans capsule called podocytes have a very specialised shape. Podocytes have finger like projections. These ensure there are gaps between cells. Fluid from the glomerulus can apss between these cells into the lumen of the Bowmans Capsule
Ultrafitration
Substances filtered in and out of blood
What is fitered out of the blood?
Blood plasma containing dissolved substances is pushed under pressure from the cappilary into the lumen of the Bowman's capsule. These substances include:
- water
- amino acids
- glucose
- urea
- inorganic ions (Na, Cl, K)
What is left in the capillary?
The blood cells and proteins are left in the capillary. The presence of proteins means that the blood has a very low water potential. This low water potential ensure that some of the fluid is retained in the blood and this contains some of the water and dissolved substances listed above. The very low water potential of blood is important to help reabsorb water at a later stage.
Formation of urine - Selective reabsorption
As fluid moves along the nephron, substances are removed from the fluid and reabsorbed into the blood. Most reabsorption occurs in proximal convoluted tubule, where 85% of filtrate is reabsorbed. All glucose and amino acids and some salts are reabsorbed along with some of the water. Reabsorption is achieved by a combination of processes. The cells lining the proximal convoluted tubule are speciallised to achieve this reabsorption.
- The cell surface membran in contact with the tubule fluid is highly folded to form microvilli. This increase the surface area for reabsoption.
- Membrane contains special co-tranbsporter proteins that transport glucose or amino acids from the tubule to the cell. This is faciliated diffusion.
- The opposite membrane of the cell, close to the tissue fluid and blood cappilaries is also folded to increase surface area. The membrane contains Na/K pumps that pump Na ions out of and K ions into the cell.
- The cell cytoplasm has many mitochondria. This indicated than an active, or energy requiring process is involved.
Selective reabsorption
As fluid moves along the nephron, substances are removed from the fluid and reabsorbed into the blood. Most reabsorption occurs from the proximal convoluted tubule. All the glucose and amino acids and some salts are reabsorbed along with some water. Reabsorbed is achieved by a combination of processes on next page. The cells lining the proximal convoluted tubule are specialised to achieve reabsorption:
- the cell surface membrane in contact with the tubule is highly folded to form microvilli. This increase surface area for reabsorption.
- This membrane also contains special co-transporter proteins that transport glucose or amino acids in association with sodium ion, from the tubule into the cell. This is faciliated diffusion.
- The opposite membrane of the cell, close to the tissue fluid and blood capillaries is also folded to increase surface area. The membrane contains Na/K pumps that pump Na out and K into the cells.
- The cells sytoplams has many mitochondria. This indicated it is an active process involved.
How reabsortion occurs
- The sodium-pottasium pumps remove sodium ions from the cells lining the proximal convoluted tubules. This reduces the concentration of sodium ions in the cell cytoplasm.
- Sodium ions are transported into the cell along with glucose or amino acid molecules by faciliated diffusion.
- As the glucose and amino acid concentrations rise inside the cell, these substances are able to diffuse out of the opposite side of the cell into the tissue fluid. This process may be enhanced by the removal of glucose and amino acids from the cells.
- From the tissue fluid these substances diffuse into the blood and are carried away
- Reabsorption of salts, glucose and amino acids reduces the water potential in the cells and increases the water potential of tubule fluid. This means that water will enter the cells and then be reabsorbed into the blood by osmosis.
- larger molecules, such as small proteins that may have entered the tubule, will be reabsorbed by endocytosis.
Water reabsorption
Each minute 125cm of fluid is siltered from the blood and enters tha nephron tubules. After selective reabsorption in the proximal convoluted tubuleabout 45cm is left. The role of the loop of Henle is to create a low water otential in the tissue of the medulla. This ensures even more water can be reabsorbed from the fluid in the collecting duct.
The loop of Henle: the loop of Henle consists of a decending limb that decends into the medulla and the accending limb which ascends back to the cortex. The arrangement of the loop of Henle allows salts to be transferred from the accending limb to the decending limb. The overall effect is to increase the concentration of salts in the tubule fluid and consequently they diffuse out from the thin walled ascending limb into the medulla tissue, giving the tissue fluid in the medulla a very low water potential.
How water is reabsorbed
As the fluid in the tubule descends deeper into the medulla its water potential becomes lower. This is due to:
- loss of water by osmosis to the surrounding tissue fluid
- diffusion of sodium and chloride ions into the tubule from the surrounding tissue fluid
As the fuid ascends back up towards to cortex its water potential becomes higher due to:
- at the base of the tubule, Na and Cl ions diffuse out of the tubule into the tissue fluid.
- higher up the tubule, Na and Cl ions are actively transported out into the tissue fluid
- the wall of the acsending limb is impermeable to water so water can not leave the tubule
- the fluid looses salts but not water as it moves up the acending limb
The arrangement of the loop of Henle is known as a hairpin countercurrent multiplier system - the arrangement of the tubule is in a sharp hairpin so that one part of the tubule passes close to the other part flowing in opposite directions. This allows exchange between the contents and can be used to create a high concentration of solutes.
The collecting duct
From the top of the ascending limb the tubule fluid passes along a short distal cnvoluted tubule where active transport is used to adjust the concentrations of various salts.
From here the fluid flows into the collecting duct. At this stage the tubule fluid still contains a lot of water (high water potential).
The collecting duct carries the fluid back down through the medulla to the pelvis. The tissue fluid in the medulla has a low water potential that becomes even lower as you go deeper.
As the tubule passes down the collecting duct water move, by osmosis, from the tubule fluid into surrounding tissue. It then enters the blood cappilaries, by osmosis, and is carried away.
The amount of water reabsorbed depends on the permeability of the walls of the collecting duct. By the time the urine reaches the pelvis it has a low water potential and the concentration of urea and salts in urine is higher than that of the blood plasma.
Osmoregulation
Osmosregulation is the control of water levels and salt levels in the body. The correct water balance between the cells and the surrounding fluids must be maintained to prevent problems with osmosis.
Water is gained from: food, water and metabolism
Water is lost in: urine, sweat, water vapour in exhaled air, faeces
If it is a cool day and you have drunk a lot of fluid you will produce a large volume of dilute urine. Alternatively, on a hot day with little water your urine will be small amounts of concentrated volume. Controlling the loss of water in urine is just one part of the osmoregulation process.
The walls of the collecting duct can be made more or less permeable depending upon needs of the body. When we need to conserve less water, the wall of the collcting duct is less permeable. On a hot day, when you need to conserve more water, the collecting duct walls are more permeable so that more water can be reabsorbed into the blood, so you will produce a smaller volume of urine.
Permeability of collecting duct
The walls of the collecting duct respond to the level of ADH in the blood. Cells in the walls have membrane bound receptors for ADH, which binds to these receptors and causes a chain of enzyme controlled reactions inside the cell. The end result of these reactions is to insert vesicles containing water permeable channels (aquaporins) into the cell surface membrane. This makes the walls more permeable to water.
If there is more ADH in the blood, more water permeable channels are inserted. This allows more water to be reabsorbed by osmosis into the blood. so less urine passes out of the body.
If there is less ADH in the blood then the cell surface membrane folds inwards to crease new vesicles that remove water permeable channels from the membrane. This makes the walls less permeable and less water is reabsorbed by osmosis into the blood so more water passes out in the urine.
Adjusting concentration of ADH
- The water potential of the blood is monitored by osmoreceptors in the hypothalumus of the brian
- These cells probably respond to the effects of osmosis. When the water potential of the blood is low, the osmoreceptors lose water by osmosis. This causes them to shrink and stimulate neurosecretory cells in the hypothalamus.
- The neurosecretory cells are speciallised nerve cells that produce and release ADH. The ADH is manufactured in the cell body of these cells, which lies in the hypothalumus. ADH flows down the axon to the terminal bulb in the posterior pituitary gland. It is stored there until needed.
- When the neruosecretory cells are stimulated they send action potentials down the axons and cause the release of ADH.
- The ADH enters the blood capillaries running through the posterior pituitary gland. It is transported around the body and acts on the cells of the collecting ducts (its target cells).
- Once the water potenital of the blood rises again, less ADH is released.
- ASH is slowly broken down - it has a half life of about 20 minutes. Therefore the ADH present in the blood is broken down and the collecting ducts will recieve less stimulation.
ADH negative feedback
Kidney failure
Kidney failure can occur for a number of reasons. The most common causes are:
- infection,
- hypertension
- diabetes mellitus.
Once the kidneys fail completely the blood is unable to remove excess water and certain water products from the blood. This includes urea and excess salts.
It is also unable to regulate the levels of water and salts in the body. This will rapidly lead to death.
Treatment of kidney failure
Treatment of kidney failure:
- Dialysis - use of a particually pemeable mebrane to filter the blood over a dialysis memrane. The dialysis membrane is a partially permeable membranethat allows the exchange of substanced between the blood and dialysis fluid. This fluid contains the correct concentrations of substances needed in blood. Any substances in excsess in the blood diffuse across the membrane into the dialysis fluid and vice versa. Dialysis must be combined with a carefully monitored diet. In haemodialysis blood from a vien is passes into a machine that contains an artificial dialysis memrane, perfrmed 3-5 times a week, where as in peritoneal dialysis (PD) the filter is the bodys own abdominal membrane. Fist a surgeon implants a permanent tube in the abdoment and solution is drained from the abdoment. It is perfromed in several consecutive session s daily at home or work.
- Kidney transplant - in a transplant the old kidneys are left in place unless they are likely to cause and infection. The donor kidneys can be from a living relative or from someone who had died. A kidney transplant is a major surgery. While under anaethetic, the surgeon implants the new organ and attaches it to the blood supply and the bladder. Many feel much better immediatly, however some patients reject the kidney as a foreign object and drugs are used to help this.
Advantages and diadvantages of transplant
Advantages:
- Freedom from time consuming dialysis
- Diet is less limited
- Feeling better physically
- A better quality of life (able to travel)
- No longer seeing oneself as chronically ill
Disadvantages:
- Need immunosupressants for the life of the kidney
- Need major surgery under a general anaesthetic
- Risks of surgery include infection, bleeding and damage to surroundsing organs
- Frequent checks for signs of organ rejection
- Side effcts: anti rejection medicines cause fluid retention and high blood pressue
Urine samples
Substances or molecules with a relative molecular mass of less than 69000 can entre the nephron. This means that any metabolic product or other substance that is in th eblood can be passed to urine as long as its small enough. If these substances are not reabsorbed further down the nephron they can be detected in urine.
Pregnancy testing: once implanted in the uterine lining, a human embryo starts secreting a pregnacy hormone called hCG. This is a relatively small glycoprotein. It can be found in the urine as early as up to 6 days after conception.Pregnancy tests are manufactured with monoclonal antibodies. The antibody is specific to hCG. Any hCG in urine attached to antibody, this causes a ***** to appear.
Testing for anabolic steroids: Anabolic steroids increase protein synthesis. This results in the build up of cell tissue in muscles. They have a half llife of 16 hours and reamin in clood for many days. They are small and enter nephron easily. Testing for anabolic steroids involves analysing a urine sample using gas chromatography. Thid id where the same is vaporised in presence of a gaseos solvent and each substance dissolved differentially in gas a stays there for a set time. This is analysed to create a chromatogram and certain drugs are identified within the sample.


Comments
No comments have yet been made