Basic life support
0.0 / 5
- Created by: Charlotte170289
- Created on: 02-01-21 14:36
Basic life support- some key terms
- Basic life support- is a set of life saving first aid skills.
- Cardic arrest- is the absence of signs of life, no pulse and no normal breathing and requires cardiopulmonary resuscitation (CPR)
- Cardio-pulmonary resuscitation (CPR) -refers to the basic first aid procedures that can be used to keep someone alive until the emergency medical services can get to the scene
- Defibrillation- is the passage of electrical current across the myocardium
- Defibrillator- is the devise used to pass the current of electricity across the myocardium
- Aerosol generating procedure (AGP)- is a medical procedure that can result in the release of airborne particles from the respiratory tract
- Personal protective equipment (PPE)- is the equipment designed to help protect a user from injury or infection
1 of 13
What is CPR all about?
- CPR can be a life saving intervention
- The public has an expectation that all clinical staff can undertake CPR (resuscitation council 2015)
- Therefore it is essential for all NHS staff to have the underpinning knowledge and skills to undertake CPR
2 of 13
Why is CPR important?
- The community response to cardiac arrest is critical to saving lives. Each year the UK ambulance services responds to approximately 60,000 cases of suspected cardiac arrest.
- Resuscitation is attempted by ambulance services in less than half of these cases (aprox 28,000). The main reasons are that either the victim has been dead for several hours or has not received bystander CPR, so by the time the emergancy services arrive the person has died. Even when resuscitation is attempted, less that 1 in 10 victims survive to go home from hospital.
- Strengthening the community response to cardiac arrest by training and empowering more bystanders to perform CPR and by increasing the use of automated external defibrillators (AEDs) at least doubles the chances of survival annd could save thousands of lives each year.
3 of 13
The chain of survival

4 of 13
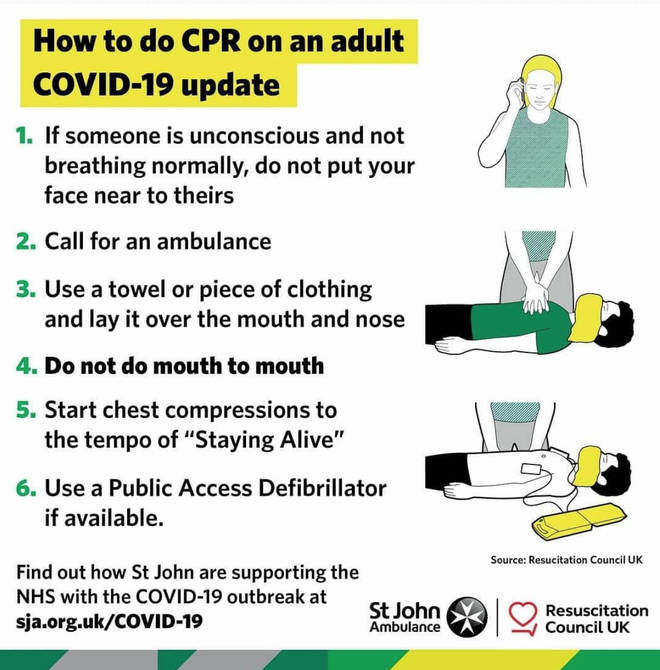
CPR and Covid 19
- Covid 19 has meant that some changes to the way we manage a cardiac arrest for both in and out of hospital
- Dring CPR, there is potential for rescuers to be exposed to bodily fluids, and for procedures (e.g. chest compressions and tracheal intubation or ventilation) to generate an infectious aerosol, therefore CPR is deemed an AGP.
- Individual healthcare organisations should carry out local risk assessments, based on the latest guidance from the RCUK/DHSC/PHE regards to HCWs to develop local guidance
- RCUK- Resuscitation council uk
- DHSC- Department of health and social care
- PHE- Public health England
- HCWs- Healthcare workers
5 of 13
Out of hospital BLS pre covid 19 and now

6 of 13
Defibrillation
- If a defibrillator becomes available after chest compressions have been commenced do not stop chest compressions to apply the defibrillator pads.
- Apply pads as indicated by the pictures
- It is most likely you will be using an automated external defibrillator (AED)- they tell you exactly what to do
7 of 13
Chest compressions
- A chest compression is a technique that manually pumps blood around a patients body.
- Place one hand on the center of the chest (the middle of the lower half of the sternum) and the other hand on top.
- Ensure high quality chest compressions at a depth of 5-6 cm and a rate of 100-120 compressions a minute.
- Allow the chest to recoil (return to the normal position) after each compression
- Minimise any interruptions to chest compressions (hands off time)
- If more then one rescuer available, rotate chest compressions every 2 minutes

8 of 13
What to do- both in and out of hospital
- Is it safe to approach?
- Look for absence of signs of life/ normal breathing
- Do not listern and feel for breath by placing your ear or cheek close to the patients mouth
- Feel for carotid pulse if trained to do so
- Call for help (999 out of hospital, 2222 in hospital)
Out of hospital
- Place a covering over the patients nose and mouth
- If an automated external defibrillator (AED) is available follow the instructions given and shock if advised.
- Begin chest compressions at a rate of 100-120 per minute at a depth of 5-6 cm
- Continue chest compressions/ defibrillation until help arrives
In hospital
- Do not perform any task or role that you have not been trained to do or without appropriate PPE.
- As a student the role will be determined by a number of factors that will be decided on an individual basis. Your role may be as a gate keeper- restricting the number of staff in an area during a cardiac arrest. You may also be a scribe writing down the events of the cardiac arrest if you feel comfortable in doing so. You may support the event by collecting equipment/ medications that may not be readily available.
9 of 13
Resuscitation council in hospital high, medium and
- In september 2020 the resuscitation council updates its guidance on the management of an in hospital cardiac arrest and the treatment, care and support is to be managaed within three pathways: High, medium and low risk.
- High risk: known or suspected Covid 19
- Medium risk: this includes patients/individuals who have no symptoms of covid 19 but do not have a covid 19 test results.
- Low risk: patients/individuals with no symptoms and a negative covid 19 test, who have self isolated prior to admission. Follow pre-covid resuscitation algorithms.
- Known os suspected covid 19 aligns with the high and medium risk categories. We therefore recommed that the covid 19 algorithms are followed and that AGP PPE continues to be used for chest compressions and advanced airway procedures for patients allocated to these two categories.
10 of 13
So what happens in hospital?
- A patient in cardiac arrest in hospital will receive advanced life support- this is provided by specially trained healthcare providers.
- CPR will be commenced but only when appropriate PPE is donned.
- A cardiac arrest call 2222 will be placed.
11 of 13
Decisions about resuscitation
- The conversations and decision-making processes around resuscitation must continue and must be individualised unless directives state otherwise.
- Conversations, and treatment escalation planning must be a priority (ReSPECT)
- Ensure "do not attempt cardiopulmonary resuscitation" (DNACPR) decisions are well documented and communicated.
12 of 13
ReSPECT
- Provides health and care professionals responding to an emergency with a summary of recommendations to help them to make immediate decisions about that persons care and treatment.
- ReSPECT can be complementary to a wider process of advance/anticipatory care planning.
- The ReSPECT process creates personalised recommendations for a person’s clinical care and treatment in a future emergency in which they are unable to make or express choices.
- These recommendations are created through conversations between a person, their familes and their health and care professionals to understand that matters to them and what is realistic in terms of their care and treatment.
- Patient preferences and clinical recommendations are recorded and a non-legally binding from which can be reviewed and adapted if circumstances change.
- The ReSPECT process can be for anyone but will have increasing relevance for people who have complex health needs, people who are likely to be nearing the end of their lives, and people are at risk of sudden deterioration or cardic arrest.
- Some people will want to record their care and treatment preferences for other reasons.
13 of 13
Related discussions on The Student Room
- Life as a student nurse at Bradford »
- The Difference between Adult Nursing, Child Nursing and Mental Health Nursing »
- 5 careers for Adult Nursing Graduates »
- Adult or child nursing? »
- Applying for university »
- Adult or children nursing degree »
- Advice »
- SLT or nursing, or both? »
- Midwifery »
- York University interview - adult nursing »
Similar Nursing resources:
0.0 / 5
0.0 / 5
0.0 / 5
0.0 / 5
0.0 / 5
0.0 / 5
0.0 / 5
0.0 / 5
0.0 / 5
0.0 / 5


Comments
No comments have yet been made