Homeostasis
- Created by: _pxmudi_
- Created on: 27-01-19 08:42
Importance of Homeostasis in Mammals
Homeostasis maintains a constant internal environment for the cells within the body.
Some of the physiological factors controlled are:
- core body temperature
- metabolic wastes (CO2 and urea)
- blood pH
- blood glucose concentration
- water potential of the blood
- concentrations in the blood of respiratory gases (O2 and CO2).
Temperature:Low temp. slow down metabolic reactions. At high temp., proteins (enzymes) denature and cannot function.
Water potential: If it decreases, water move out of cells, causing metabolic reactions in the cell to slow/stop. If it increases, water enter the cell, causing it to swell and burst.
Glucose concentration: Lack of it causes respiration to slow/stop, depriving cell's energy source. Too much cause water to move out by osmosis, disturbing cell's mechanism.
Principles of Homeostasis
Requirements for homeostasis:
- receptors - detect specific changes in the environment
- control centres - act to direct impulses to the place where a response can be made (eg: brain and spinal cord)
- effectors - perform the appropriate response (eg: muscles and glands)
- a negative feedback process.
The receptor detects stimuli that are involved with the condition being regulated.
These receptors send information to a central control (the input), and the central control instructs an effector to carry out an action (the output).
Negative Feedback
Negative feedback- a process in which a change in some parameter brings about processes which move its level back towards normal again.
It brings the internal environment back to the set point (and not beyond this point).
- Factor rises above set point.
- Receptors sense change in factor.
- Effectors recieve information from receptors.
- Effectors act to decrease factor.
- Factor falls below set point.
- Receptors sense change in factor.
- Effectors recieve information from receptors.
- Effectors act to increase factor.
- Factor rises above set point...and so on.
The factor fluctuates around the set point as this mechanism keep changes in the factor within narrow limits.
It minimises the difference between the actual value of the factor and the ideal value.
Roles of the Nervous System and Endocrine System
Nervous System
- When osmoreceptors detect a decrease in water pot., nerve impulses are sent along the neurones to where they terminate in the posterior pituatary gland.
Endocrine System
- If the core temp. decreases, the secretion of adrenaline increases.
- When the environmental temp. decreases gradually, the hypothalamus releases a hormone which activates the anterioir pituatary gland to release TSH. TSH stimulates the thyroid gland to secrete the hormone thyroxine.
- ADH is a hormone which reduces the loss of water in urine.
- The homeostatic control of blood glucose conc. is carried out by 2 hormones; glucagon and insulin.
- Adrenaline increases blood glucose conc.
Deamination of Amino Acids
Deamination is the breakdown of excess amino acids in the liver, by the removal of the amine group.
Highly toxic ammonia and a useful keto acid (eg: respiration, conversion for energy storage) are formed.
Ammonia is immediately converted immediately to urea, which is less soluble and less toxic.
Formation of Urea
Urea:
- not poisonous
- has a high solubility
- gets filtered easily as the molecules are very small.
Urea is the main nitrogenous excretory product.
Small quantities of creatinine and uric acid are also produced.
Gross Structure of the Kidney
The kidney is covered by a fairly tough capsule, beneath which lies the cortex. The cortex is made of fibrous connective tissue. It contains glomeruli and nephrons.
The central area is made up of the medulla, composed of tubular parts of the nephrons and blood vessels, together forming renal pyramids.
All the pyramids project into the pelvis which leads into the ureter.
Each kidney recieves blood from a renal artery, and returns blood via a renal vein.
Detailed Structure of the Nephron - I
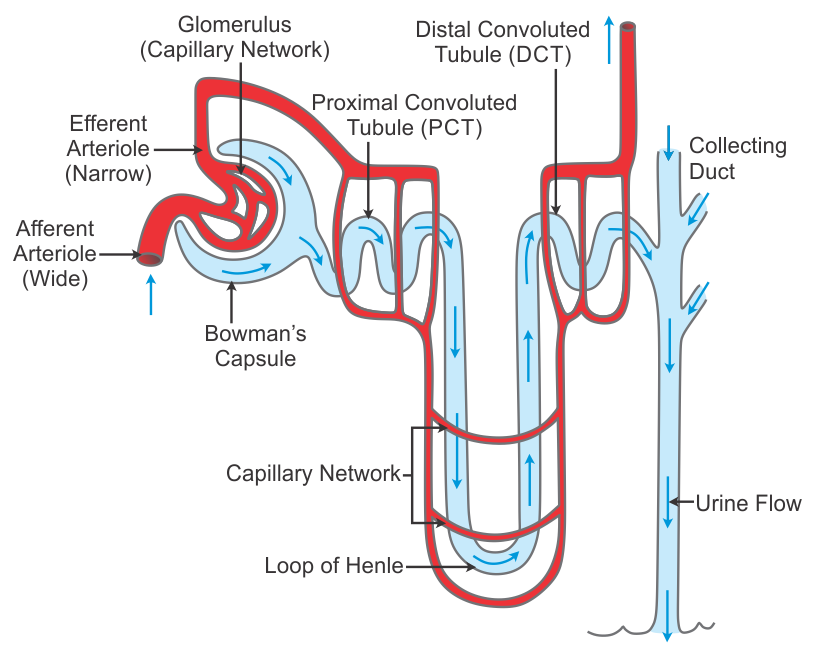
Detailed Structure of the Nephron - II
A nephron is a tubular structure.
One end of the tube forms a cup-shaped structure called a Bowman's capsule (in cortex), which surrounds a tight network of capillaries called a glomerulus.
The tube runs towards the medulla forming the PCT, and then a long hairpin loop (in medulla) called the loop of Henle. It then runs back up forming the DCT.
Many convoluted tubules of a number of nephrons open into one collecting duct that opens into the pelvis which opens to the ureter.
The collecting duct and capillaries around it make a renal pyramid.
Each glomerulus is supplied with blood by a branch of the renal artery called the afferent arteriole. The capillaries of the glomerulus rejoin to form an efferent arteriole.
3cm long. The length of all tubes in kidney is about 120km. This provides a large surface area for the exchange of particles.
Ultrafiltration - Structure
This involves filtering small molecules, including urea, out of the blood and into the Bowman's capsule.
The blood in the glomerular capillaries is separated from the lumen of the Bowman's capsule by 2 cell layers and a basement membrane.
- Endotheliumof capillary - Has a lot of gaps in it.
- Basement membrane- Made up of a network of collagen and glycoproteins. Stops large protein molecules (with a relative molecular mass of 69000 or more) from getting through, and so cannot escape from the glomerular capillaries. Acts as a filter.
- Epithelium cells of Bowman's capsule - Have many tiny finger-like projections with gaps in between them called podocytes.
Ultrafiltration - Process
The blood pressure inside the glomerulus is high beacuse:
- The renal artery contains blood at very high pressure which enters the glomerulus via the short afferent arteriole.
- The efferent arteriole has a smaller diameter than the afferent arteriole.
The high pressure forces small molecules through the filter, from the blood in the glomerular capsule across the Bowman's capsule and into the nephron. The fluid formed in this way is the glomerular filtrate.
The interlocking of the podocyte extension creates gaps for the filtrate to pass between the cells. This means that the filtrate does not pass through the cells of either the glomerulus or the Bowman's capsule.
Substances that can pass through the basement mem. -- water, glucose, amino acids, fatty acids, urea, minerals, small proteins.
Substances that cannot pass thorugh -- red blood cells, white blood cells, platelets, large plasma proteins.
Ultrafiltration - Factors Affecting Fil. Rate
Glomerular filtration rate - the rate at which the fluid filters from the blood in the glomerular capillaries into the Bowman's capsule.
What makes the fluid filter through so quickly is the differences in water potential between the plasma in glomerular capillaries and the filtrate in the Bowman's capsule.
Inside the capillaries in the glomerulus, the blood pressure is relatively high, causing a head of pressure in the glomerulus.
However, conc. of solutes in blood plasma > conc. of solutes in filtrate in Bowman's capsule. This is because the plasma proteins are too big to get through and remain in the blood.
Water pot. in blood capillaries < Water pot. of the filtrate in Bowman's capsule
Overall, the effect of differences in pressure outweighs that of the differences in solute conc. So water continues to move down the water pot. gradient from blood into the capsule.
- Water pot. is lowered by the prescense of solute, and raised by high pressures.
Selective Reabsorption - Adaptations of PCT cells
The lining of PCT is made of a single layer of cuboidal epithelial cells.
Adaptations:
- microvilli - to increase the surface area
- tight junctions - so that fluid cannot pass between the cells; all substances that are reabsorbed must go through the cells
- many mitochondria- to provide energy for Na+/K+ pumps
- co-transporter proteins.
Selective Reabsorption - Process
- Na+/K+ pumps in the basal mem. of PCT cells decrease the conc. of Na+ in the cytoplasm.
- Very close nearby, the blood plasma rapidly removes absorbed Na+, Cl-, glucose and amino acids. This helps further uptake from the lumen of the tubule.
- Na+ moves passively into the cell down its conc. gradient. It moves using protein co-transporter molecules in the mem., which bring in glucose and amino acids at the same time.
- The removal of solutes increases the water pot. of filtrate. The movement of solutes into the cells and then into the blood decreases the water pot. there.
- Therefore, a water pot. gradient exists between filtrate and blood.
- Water moves down this gradient through the cells and into the blood. This water and reabsorbed solutes are carried back into the circulation.
- Conc. of urea in the filtrate is higher than that in the capillaries, so it diffuses passively through the cells of the PCT and into the blood.
- Uric acid and creatinine are not reabsorbed.
- Creatinine is actively secreted by the cells of the PCT into its lumen.
Selective Reabsorption - L. of Henle and C. Duct
The function of these loops is to create a very high conc. of Na+ and Cl- in the tissue fluid in the medulla. So a lot of water is reabsorbed from the fluid in the c. duct as it flows through the medulla.
ascending limb- not permeable to water descending limb - permeable to water and Na+/Cl-
- Na+/Cl- are actively transported out of ascending limb. This decreases the water pot. in the tissue fluid and increases inside the ascending limb.
- Water moves out from descending limb and Na+ and Cl- diffuse into the limb, down their conc. gradient.
- By the time the fluid has reached the bottom of the loop, it contains less water and many ions.
- At the bottom of the ascending limb, ions are transported actively out of the limb. As the fluid continues up the limb, loosing ions all the time, it becomes less concentrated.
- The cells lining the ascending limb and collecting ducts are permeable to urea, which diffuses into the tisuue fluid. Now, urea is also concentrated in the medulla.
- The tissue fluid around collecting ducts have high solute conc. and low water pot. Water therefore move out of the collecting duct by osmosis, until the water pot. of urine is equal to the water pot. of the tissue fluid in medulla. The degree of this is controlled by ADH.
Selective Reabsorption - Counter-Current Multiplie
Having the 2 limbs of the loop of Henle running side by side, with the fluid flowing down in one and up in the other, enables the maximum conc. of solutes to be built up both inside and outside the tube at the bottom of the loop.
This mechanism is called a counter-current multiplier.
Selective Reabsorption - DCT and C. Duct
- Na+ are actively pumped from the tubule fluid to the tissue fluid, where they pass into the blood.
- K+ are actively transported into the tubule.
Osmoregulation
Osmoregulation- control of the water pot. of body fluids.
Role of hypothalamus
The water pot. of the blood is constantly monitored by osmoreceptors in the hypothalamus.
Role of posterior pituitary gland
When these detect a decrease in water pot. below the set point, nerve impulses are sent along the neurones to where they terminate in the posterior pituitary gland. These impulses stimulate the release of antidiuretic hormone (ADH) to the blood.
Role of ADH
ADH reduces the loss of water in urine by making the kidney reabsorb as much water as possible. The cells of the collecting duct are the target cells.
Low ADH - c. duct wall impermeable to water. High ADH - c. duct wall permeable to water.
Osmoregulation - How ADH In. Permeability
- ADH binds to receptors in the cell surface of the cells lining the c. duct.
- This activates a series of enzyme-controlled reactions, ending with the production of an active phosphorylase enzyme.
- The phosphorylase causes vesicles, surrounded by mem. containing aquaporins, to move to cell surf. mem.
- The vesicles fuse with the cell surf. mem.
- Water move freely through the mem., down its water pot. gradient, into the conc. tissue fluid and blood plasma in the medulla of the kidney.
Regulation of Blood Glucose Conc.
The homeostatic control of blood glucose conc. is carried out by 2 hormones secreted by endocrine tissue in the pancreas. The islets of Langerhans contain 2 types of cells:
- alpha-cells secrete glucagon
- beta-cells secrete insulin.
These cells act as the receptors and the central control; the hormones coordinate the actions of the effectors.
- High blood glucose conc. - The receptors detect rise in blood glucose. Less glucagon and more insulin secreted. Effectors: 1.No glycogen breakdown occurs in liver cells. 2.Increased uptake and use of glucose in liver, muscle and fat cells.
- Low blood glucose conc. - Receptors detect fall in blood glucose. More glucagon, less insulin. Effectors: 1.Liver cells break down glycogen to glucose. 2.Reduced uptake of glucose in liver, muscle and fat cells.
Role of Cyclic AMP as a Sec. Messenger
Second messengers are intracellular signaling molecules released by the cell in response to exposure to extracellular signaling molecules—the first messengers.
The binding of glucagon to a receptor activates a G protein, that in turn activates an enzyme within the mem. that catalyses the conversion of ATP to cyclic AMP.
cAMP is used for intracellular signal transduction, such as transferring into cells the effects of hormones like glucagon and adrenaline, which cannot pass through the plasma membrane. It is also involved in the activation of protein kinases.
Control of Blood Glucose by Adrenaline
Hormone-Receptor interaction at the cell surface
Adrenaline binds to different receptors on the surface of liver cells. This activates a G protein that in turn activates an enzyme.
Formation of cyclic AMP which binds to kinase proteins
This active enzyme catalyses the conversion of ATP to cyclic AMP, which is a second messenger. Cyclic AMP activates kinase proteins.
An enzyme cascade involving activation of enzymes by phosphorylation to amplify the signal
The kinase proteins activate an enzyme cascade that activates other enzymes by adding phosphate groups to them in a process known as phosphorylation. This leads to the activation of many molecules of glycogen phosphorylase that break down glycogen.
Operation of Dip Sticks
Dip sticks can be used to test urine for pH, glucose, ketones and protein.
Dip sticks for detecting glucose contain the enzymes glucose oxidase and peroxidase, immoblilised on a small pad at one end of the stick.
- The pad is immersed in urine and if it contains glucose, glucose oxidase catalyses a chemical reaction in which glucose is oxidised to glucanolactone. Hydrogen peroxide is also produced.
- Peroxidase catalyses a reaction between hydrogen peroxide and a colourless chemical in the pad to form a brown compound.
- The resulting colour is matched against a colour chart indicating diff. conc. of glucose. The more glucose that is present, darker the colour.
Problems: 1) Do not indicate the current blood glucose conc., but rather the conc. in the period of time while urine was collecting in the bladder. 2) Does not provide quantitative results.
Operation of Biosensors
A biosensor is a device which uses a biological material, such as an enzyme, a cell or an antibody to detect or measure a chemical compound. The reaction between the biological material and the chemical being measured brings about a change, which is converted to an electrical signal. The electrical signal is then amplified to give a read-out on a digital display.
- A biosensor uses a pad impregnated with glucose oxidase.
- A small sample of blood is placed on the pad which is inserted into the machine.
- Glucose oxidase catalyses the reaction to produce glucanolactone and at the same time a tiny electric current is generated.
- The current is detected by an electrode, amplified and read by the meter which produces a reading for blood glucose conc. within seconds. The more glucose, greater the reading.
Advantages: 1) Can measure the blood glucose conc. rather than detecting only the presence of glucose in urine. 2) Allows quantitative readings to be taken.
Urine Analysis used in Diagnosis - I
Glycosuria (high blood glucose levels)
Causes: 1.The level of blood glucose is so high that the renal tubules are unable to reabsorb all that is presented. 2.A failure of the tubules to reabsorb all glucose at a level where this should be possible; renal glycosuria.
The level of blood glucose at which it spills into the urine is called the renal threshold. If glycosuria occurs because a normal renal threshold has been exceeded, this is usually indicative of impaired glucose tolerance or diabetes mellitus.
High protein levels in urine (proteinuria/albuminuria/microalbuminuria)
Most protein molecules are too large to be filtered, but these are reabsorbed in the PCT, broken down and the amino acids absorbed into the blood.
It is not unusual for some protein to be present in urine for short periods, such as during high fever, after vigorous exercise and during pregnancy. However, large quantities/long term presence of protein in urine indicates that there may be a disease affecting the glomeruli or a kidney infection. It is also associated with high blood pressure.
Urine Analysis used in Diagnosis - II
Urine ketones
Ketones are produced by the liver as part of fatty acid metabolism.
In normal states, ketones will be completely metabolised so that very few/no ketones will appear in urine. If the body cannot get enough glucose for energy it will switch to using body fats, resulting in an increase in ketone production, making them detectable in blood and urine.
High ketone levels in urine may indicate diabetes mellitusor starvation.
Opening and Closing Rhythms of Stomata
Stomata control the entry of CO2 into leaves.
Opening during the day maintains the inward diffusion of CO2 and the outward diffusion of O2. It also allows the outward diffusion of water vapour in transpiration.
The closure of stomata at night when photosynthesis cannot occur reduces rates of transpiration and conserves water.
Stomata open in response to;
- increasing light intensity
- low CO2 conc. in the air spaces.
Stomata close in response to;
- darkness
- high CO2 conc. in air spaces
- low humidity
- high temp.
- water stress.
Guard Cells & Opening and Closing of Stoma
Each stomatal pore is surrounded by 2 guard cells.
Guard cells open stomatal pores when they gain water to become turgid, and close stomatal pores when they lose water and become flaccid.
How a stoma is opened
- ATP-powered proton pumps in the cell mem. actively transport H+ out of the guard cell.
- The low H+ conc. and neg. charge inside the cell causes K+ channels to open. K+ diffuses into the cell down an electrochemical gradient.
- The high conc. of K+ inside the guard cells lowers the water pot.
- Water moves in by osmosis, down a water pot. gradient.
- The entry of water increases the volume of guard cells, so they expand. The thin outer wall expands most, so the cells curve apart.
Stomata close when H+ pump proteins stop and K+ leave the guard cells. The water pot. gradient in the opp. direction causes water to leave the guard cells so that they become flaccid and close the stoma.
Role of Abscisic Acid (ABA)
ABA can be found in every part of the plant, and is synthesised in almost all cells that possess chloroplasts/amyloplasts.
ABA coordinates responses to stress; a stress hormone. In conditions of water stress, ABA is produced to stimulate stomatal closure.
Inhibition of proton pumps
Guard cells have ABA receptors on their cell surf. mem. When ABA binds, it inhibits the proton pumps to stop H+ being pumped out.
Stimulating the movement of Ca2+ into guard cells
ABA stimulates the movement of Ca2+ into the cytoplasm through the cell surf. mem. and tonoplast. Ca acts as a sec. messenger to activate channel proteins to open that allow neg. charged ions to leave the guard cells.
Ca2+ also stimulates the closure of the K+ channel proteins.
The loss of ions raises the water pot., water moves out, gu. cells turn flaccid and stoma close.
Comments
No comments have yet been made